Summary:
- 44% of patients with plantar fasciitis will have pain 15 years after the original diagnosis.
- The most common treatment protocols, including orthotics, corticosteroids, and short-term stretches have not been proven to alter long-term outcomes.
- The majority of patients with plantar fasciitis present with weakness of the peroneal and intrinsic arch muscles, and exercises targeting these muscles may reduce chronicity.
- Tightness in the medial head of the gastrocnemius correlates strongly with the development of chronic plantar fasciitis, and a specific high-volume stretching routine has recently been proven to lengthen the medial gastrocnemius by structurally changing its muscle fibers. These length gains persist even after a period of detraining.
Plantar fasciitis is a degenerative condition in which repetitive microtrauma causes a structural breakdown of the connective tissue in the plantar fascia and/or neighboring muscles. In the United States alone, more than 1 million people receive treatment for plantar fasciitis annually (1). Until recently, it was assumed the typical plantar fascial injury lasted about three months, and that only about 10% of affected individuals developed chronic heel pain. Unfortunately, a 2018 study out of Denmark confirmed that plantar fasciitis is far more difficult to get rid of than people originally thought (2). Using ultrasonography to evaluate 174 patients over a 15-year period, the authors determined that 80% of plantar fascial patients had symptoms 12 months after the original injury, 50% had symptoms at five years, and a startling 44% of the people studied had symptoms 15 years after the onset of their plantar fascial injury.
In my opinion, the terrible long-term outcomes reported in this study can be traced directly to the poor quality of care the typical plantar fascial patient receives. The classic example of this is the prescription of foot orthotics to manage plantar fascial pain. Because early research suggested that plantar fasciitis resulted from excessive foot pronation, the vast majority of plantar fascial patients received foot orthotics to limit excessive pronation. More recent research confirms that neither high nor low arches have any correlation with the development of plantar fasciitis (3), questioning the belief that people with plantar fasciitis should be treated with orthotics. While some studies show both custom and over-the-counter orthotics provide short-term relief of plantar fasciitis, long-term effectiveness of orthotic intervention has never been proven (4). Even worse, recent research shows that both short and long-term orthotic use can cause significant weakening of the intrinsic muscles of the arch (5,6), potentially setting the stage for the development of chronic plantar fascial pain.
Another popular treatment intervention for plantar fasciitis is corticosteroid injections. In theory, microtrauma at the origin of the plantar fascia causes chronic inflammation, which creates a pain cycle that can be blocked with corticosteroid injections. In a 2017 literature review evaluating the efficacy of corticosteroid injections, David et al. (7) determined that compared to placebo injections, corticosteroids slightly improved symptoms for the first four weeks, but not thereafter. Furthermore, these authors state the risks associated with steroid injections (e.g., weakening of the connective tissue) are underreported and that “higher risks cannot be ruled out.” The conclusions of this meta-analysis were not surprising because for more than 20 years now, research has consistently shown that plantar fasciitis is a chronic degenerative condition, not an inflammatory reaction.
In an attempt to understand the true causes of plantar fasciitis, Sullivan et al. (3) took 202 people with plantar heel pain and compared them to 70 asymptomatic control participants. The authors evaluated a wide range of causes for heel pain, including body mass index, foot and ankle muscle strength, calf endurance, calf tightness, arch height, occupational standing time, and exercise level. As with prior research, arch height had no connection with the development of plantar fasciitis. Rather, the factors most likely to be associated with the development of plantar fasciitis were weakness of the peroneal and intrinsic arch muscles, and calf inflexibility. Surprisingly, peroneal weakness was the strongest predictor of the development of plantar fasciitis.
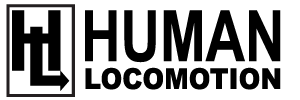
Since reading this paper a few years ago, I started routinely prescribing peroneal exercises when treating patients with plantar fasciitis and have noticed significant improvements in long-term outcomes. Strengthening the peroneus longus is especially effective when treating plantar fasciitis because this muscle creates a downward pull on the first metatarsal, increasing pressure borne by the inner forefoot thereby offloading the plantar fascia (Fig. 1A). Strengthening the intrinsic arch muscles is also important because these muscles, particularly flexor digitorum brevis, create a compressive force that prevents the plantar fascia from being stretched excessively (Fig. 1B). This is important because the plantar fascia has an extremely limited ability to elongate, so any force applied to the plantar fascia gets transmitted directly into the plantar fascia’s attachment to the calcaneus. A strong flexor digitorum brevis can prevent this from happening by absorbing tensile strain that would normally go into the plantar fascia. Lastly, calf tightness causes chronic plantar fascial injury as it results in a premature lifting of the heel during pushoff, transferring an excessive amount of force through the Achilles into the attachment of the plantar fascia (Fig. 1C). Restoring calf flexibility is one of the most important things you can do to prevent a plantar fascial injury from going chronic.
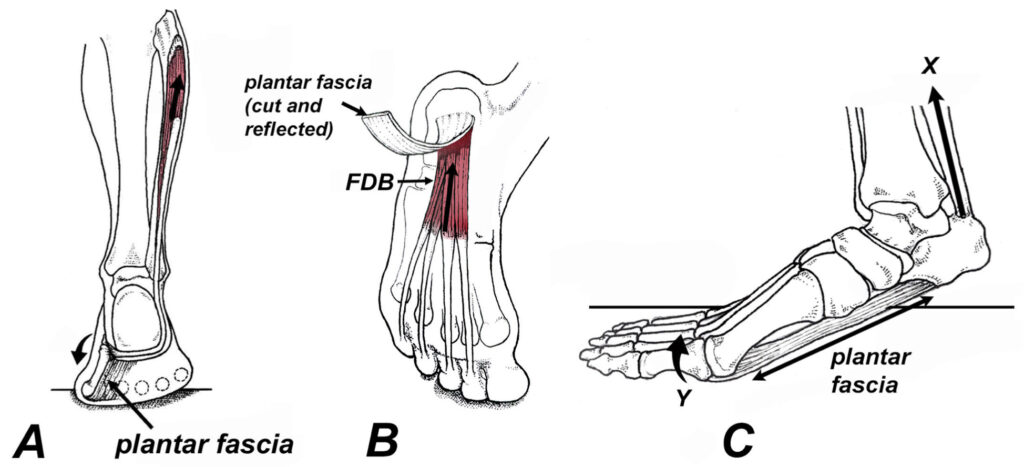
Fig. 1. (A) The peroneus longus muscle runs from the outside of the leg and attaches to the inner forefoot. Contraction of this muscle pulls the first metatarsal down (curved arrow), which offloads the plantar fascia by stabilizing the inner forefoot. (B) During pushoff, a strong flexor digitorum brevis (FDB) creates a pulling force (arrow) that prevents the plantar fascia from being stretched excessively. (C) When the calf muscles are tight, the heel leaves the ground pre- maturely (X) as the toes begin to move upward (Y). These two actions pull the plantar fascia into different directions setting the stage for chronic plantar fasciitis.
Prior to the research by Sullivan et al. (3), peroneal and toe strengthening exercises were rarely prescribed for the treatment and prevention of plantar fascial pain. In fact, I doubt a single person in the 2018 study from Denmark were told to strengthen their peroneals and/or toe flexors. In my experience, the easiest way to strengthen both the peroneals and intrinsic arch muscles is with the ToePro exercise platform (Fig. 2). Although other techniques are available, this simple home platform works the peroneals and intrinsic arch muscles at the same time thereby increasing patient compliance. To enhance strength gains, the platform is designed to keep muscles in their lengthened positions, which causes a fourfold increase in the rate of muscle development (8). A 2019 study performed at Temple University (9) showed that just six weeks of training on this exercise platform produced a measurable increase of force beneath the medial forefoot while walking (possibly from increased activation of peroneus longus) and increased toe strength as measured with toe dynamometry.
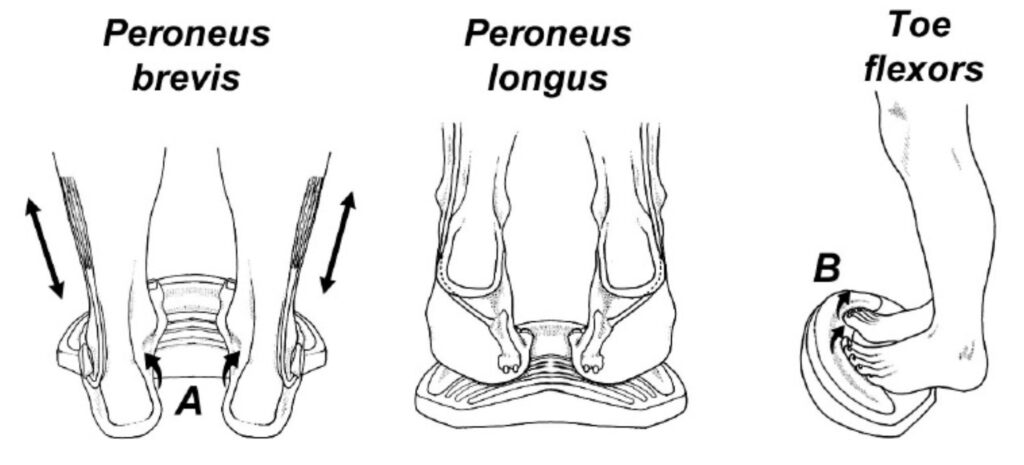
Fig. 2. The ToePro exercise platform angles down on each side to exercise the peroneal muscles in their lengthened positions (arrows in A). Also, the forward crest places the toe flexors in their lengthened positions, allowing for improved strength gains in the toes (B) and posterior calf muscles.
While increasing peroneal and arch strength is relatively simple, restoring flexibility to the calf is surprisingly difficult. As with other interventions, calf stretches have occasionally shown good outcomes for the management of plantar fasciitis, but long-term results have been questionable. In order to improve outcomes associated with stretching, it is important to understand exactly which muscle groups are responsible for the development of plantar fasciitis, and which stretching protocols produce long-term length changes in those muscles.
More than 20 years ago, DiGiovanni et al. (10) confirmed that isolated contracture in the gastrocnemius muscle alone correlated strongly not just with plantar fasciitis, but with a wide range of other foot injuries. In 2021, Pearce et al. (11) demonstrated a strong correlation between the degree of gastrocnemius tightness and the severity of heel pain in plantar fascial patients. What I find most interesting about gastrocnemius contracture is that it is not the entire gastrocnemius muscle that is responsible for producing plantar fascial pain, it is specifically the medial head of the gastrocnemius (Fig. 3). This statement is supported by the fact that surgical release of the medial gastrocnemius produces an immediate 13 degree increase in ankle dorsiflexion (12). In their 2021 review of the literature, Arshod et al. (13) confirm that surgical release of the medial gastrocnemius dramatically reduces chronic plantar fascial pain, producing better outcomes than when the plantar fascia is actually cut (plantar fasciotomy).
The circled area A is especially prone to tightening.
Although the mechanism explaining why the medial gastroc is so much tighter than the lateral gastroc is unclear, it may have something to do with the role these two muscles play in maintaining balance while standing. In an interesting study evaluating muscle activity present during static stance, researchers from British Columbia determined the medial gastroc works almost constantly during static stance to prevent falls by limiting forward displacement of the center of mass (14). This is in contrast to the lateral gastrocnemius, which is completely inactive during static stance and plays no role in maintaining postural control. According to Vladimir Janda (15), postural muscles tighten significantly faster than non-postural muscles, possibly explaining why the medial head is significantly tighter than the lateral head of the gastrocnemius. The authors of the study point out that while many muscles of the body contain multiple heads (e.g., the quadriceps, biceps, and triceps), only the medial and lateral head of the gastroc have such dramatically different recruitment patterns.
Rather than treating chronic plantar fasciitis by surgically sectioning the medial gastrocnemius muscle (or worse, cutting the plantar fascia), a less invasive approach is to lengthen the medial gastrocnemius with specific stretches. Until recently, experts suggested that it is physically impossible to lengthen a muscle by stretching, as countless studies have shown that stretches produce only temporary improvements in flexibility and they in no way actually lengthen the muscle. Fortunately, researchers from Greece and Austria (16) noticed that prior to 2021, virtually all studies on the effects of stretching incorporated short-term stretching protocols in which stretches were performed for relatively short periods of time.
These authors theorized that a high-volume stretching routine performed for an extended length of time would not only increase ankle range of motion, but increase strength and performance. The authors took 21 female athletes and had them perform 2 sets of 6 straight and bent knee calf stretches, 5 times per week for 12 weeks. At the start of the study, each stretch was held for 45 seconds and the length of time each stretch was held was increased by 15 seconds every three weeks. Total stretch duration was 9 minutes the first three weeks, and 18 minutes for the final three weeks. At the start and the end of the study, the authors used high resolution photographs to measure ankle dorsiflexion, and ultrasonography was used to create panoramic sonograms to evaluate muscle fiber length and muscle cross-sectional area. Vertical jump height was also measured pre-and post-intervention by having the athletes perform a one-leg countermovement jump.
When the study was completed, the range of ankle dorsiflexion increased by 22%, muscle fiber length of the medial gastrocnemius increased 11%, cross-sectional area increased 23%, and one-legged jump height increased
27%. The fact that these stretches specifically lengthened the medial gastrocnemius is particularly important for the management of plantar fasciitis, as lengthening the medial gastroc has a long history of successfully resolving plantar fascial pain. Importantly, the authors note that the improved range of ankle motion was maintained even following detraining.
The clinical implication of this important paper is that short-term stretching protocols typically prescribed to treat plantar fasciitis need to be replaced with the high-volume stretching routines used in this study. In addition to increasing muscle cross-sectional area and improving jump height, the long-term stretching routine actually added more muscle fibers (sarcomeres) to the existing muscles, for the first time ever showing that it is possible to physically lengthen a muscle with stretches. This research has implications not just for the management of chronic plantar fasciitis, but for decreasing injury risk and/or improving performance in a wide range of activities.
If you’ve been dealing with chronic plantar fascial pain, or if you just want to make your muscles longer and stronger, I highly recommend the stretches and exercises illustrated in figure 4. According to the latest research, the prolonged stretches used in this protocol not only increase muscle length, they increase muscle volume and athletic performance. The entire routine takes a little over 10 minutes per day to perform, but if you know the frustration of dealing with chronic plantar fascial pain, the that will seem like a small price to pay to get rid of this nagging injury once and for all.
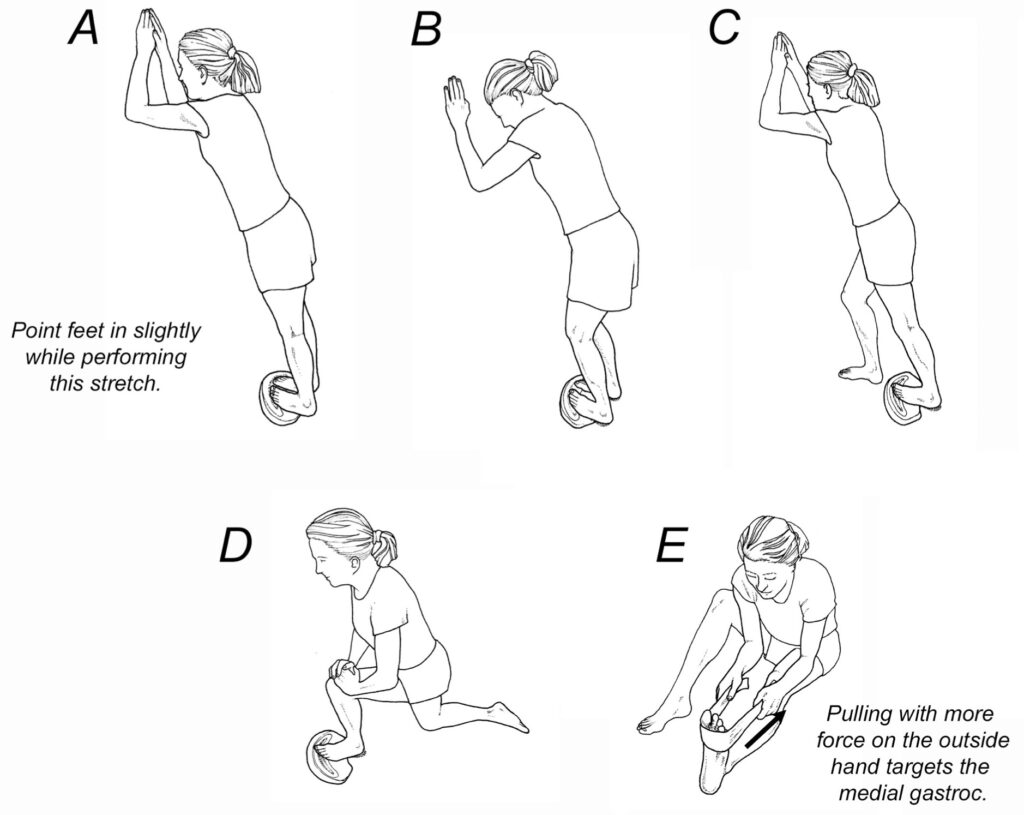
Fig. 4. Plantar fascial home stretching protocol. Before beginning the stretches, massage the medial head of the gastroc for 2 minutes using a foam roller or a percussion massage tool. The stretches can be performed using a ToePro or a slant board. To lengthen the medial gastrocnemius, hold stretches A through E for 60 seconds each and repeat twice daily. The stretches should be held to the point of mild discomfort and the stretch intensity is maintained by leaning forward so the heel leaves the ground slightly. The entire routine should be performed five times per week for 12 weeks. After that, the stretches should be performed once or twice a week. Maintenance stretching typically does not require prolonged hold times, and each stretch can be held for 30 seconds and performed once a day.
References:
- Riddle D, Schappert S. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25:303-310.
- Hansen L, Krogh T. Ellingson T, et al. Long-term prognosis of plantar fasciitis. A 5- to 15-year follow-up study of 174 patients with ultrasound examination. Orthop J Sportsmed 2018; 6:1-9.
- Sullivan J, et al. Musculoskeletal and activity-related factors associated with plantar heel pain. Foot & Ankle Int. 2015;36:37-45.
- Anderson J, Stanek J. Effect of foot orthoses as treatment for plantar fasciitis or heel pain. J Sport Rehab. 2013;22: 130-6.
- Protopapas K, Perry S. The effect of a 12-week custom foot orthotic intervention on muscle size and muscle activity of the intrinsic foot muscle of young adults during gait termination. Clinical Biomech. 2020;78.
- McClinton S, Collazo C, Vincent E, et al. Impaired foot plantarflexor muscle performance in individuals with plantar heel pain and association with foot orthosis use. J Orthop Sports Phys Ther. 2016;46:681-689.
- David J, Sankarapandian V, Christopher P, et al. Injected corticosteroids for treating plantar heel pain in adults. The Cochrane Database of Systematic Reviews. 2017;(6): CD009348.
- Goldmann J, Sanno M, Willwacher S, et al. The potential of toe flexor muscles to enhance performance, Journal of Sports Sciences. 2012;31:424-433.
- Song J, Gorelik S, Husang D, Morgan T. Effects of eccentric exercises on foot structure, balance, and dynamic plantar loading. Gait Study Center, Temple University School of Podiatric Medicine. 2019, in press.
- DiGiovani C, Kuo R, Tejwani N, et al. Isolated gastrocnemius tightness. JBone Joint Surg. 2002;(84A):962-971.
- Pearce C, Seow D, Lau B. Correlation between gastrocnemius tightness and heel pain severity in plantar fasciitis. Foot Ankle Int. 2021;42:76-82.
- Chimera NJ, Castro M, Manal K. Function and strength following gastrocnemius recession for isolated gastrocnemius contracture. Foot Ankle Int. 2010;31:377-384.
- Arshad Z, Aslam A, Razzaq M, et al. Gastrocnemius release in the management of chronic plantar fasciitis: a systematic review. Foot and Ankle Int. 2021.
- Heroux M, Dakin C, Luu B, et al. Absence of lateral gastrocnemius activity and differential motor unit behavior and soleus and medial gastrocnemius during standing balance. J Appl Physiol 2014;116:140-148.
- Janda V. Muscle testing and function. Sydney: Butterworths, 1983:230-4.
- Panid L, Bogdanis G, Terziz G, et al. Muscle architectural and functional adaptations following 12-weeks of stretching in adolescent female athletes. Frontiers in Physiology. July 2021; 12: 701338.