In any given year, nearly 40% of senior citizens aged 70 and over will fall at least once (1). Each fall significantly increases the risk of not only sprains, strains, and contusions, but also fractures. The resultant injuries often begin a downward spiral of weakness and frailty. Putting aside the emotional toll of dealing with falls, the financial costs are staggering. In the US alone, the cost of providing healthcare for seniors following falls is roughly $30 billion annually (2).
Surprisingly, the single best predictor of a senior citizen falling is toe strength. In a prospective study of 300 older adults, Mickle et al. (3) discovered that non-falling seniors had 20% more toe strength than the seniors who fell. Interestingly, there was no difference in quadriceps or ankle strength between the fallers and the non- fallers, confirming that toe weakness, not generalized weakness, is responsible for the falls. Unfortunately, toe weakness is extremely common in senior citizens: compared to their younger peers, older adults have toe strength declines of more than 35%, which greatly increases the risk of falling (4).
To understand the connection between toe strength and falling, stand with your arms at your side while keeping your hips and shoulders in a straight line. Now, maintain this straight alignment while you lean forward: notice how your toes, especially your big toes, immediately push down into the floor to protect against a forward fall. The distance you can lean forward while keeping your balance is called the anterior fall envelope, and the seniors at greatest risk of falling have a small anterior envelope. Strengthening the toes reduces the risk of falling by allowing you to control that subtle forward lean that begins while reaching forward to grasp an object, and while beginning to walk forward (the two most common times for a fall to occur).
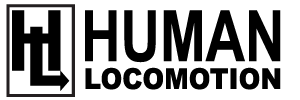
A simple exercise to increase the anterior fall envelope and reduce the risk of falling is to have your patient perform the Vele Forward Lean Maneuver (Fig. 1). To perform this maneuver, have the patient stand in front of a wall while keeping their hips and torso straight. Next, while maintaining this aligned position, have the patient slowly lean forward while aggressively pushing their toes down into the ground. The downward force with the toes decelerates forward motion of the torso, gradually increasing the size of the anterior fall envelope. I typically have the patient hold this position for 5 seconds before pushing their body back to a vertical position by pressing down vigorously with their toes. This maneuver is repeated 20 times daily.
The standing patient is instructed to maintain spinal and lower extremity alignment while leaning forward as far as possible. The degree of forward lean is controlled by pushing down firmly with the toes.
This test can be modified by having the patient place a weight in a reinforced grocery bag while performing the forward lean. The weight can be transferred from one hand to the other. As noted by Hill et al. (5), holding a weight equaling 5% body mass in the left hand, then right hand, then both hands, produces significant reductions in postural sway in older adults. Remember, a large number of falls occur while the person is leaning forward to grasp an object. Switching the weight from one hand to the other every 5 seconds while leaning forward duplicates the movements that often initiate a fall, and the increased toe strength associated with performing this exercise can produce significant increases in stability when reaching for objects. To lessen the risk of falling while performing this exercise, make sure the patient is standing in front of a wall or stable surface.
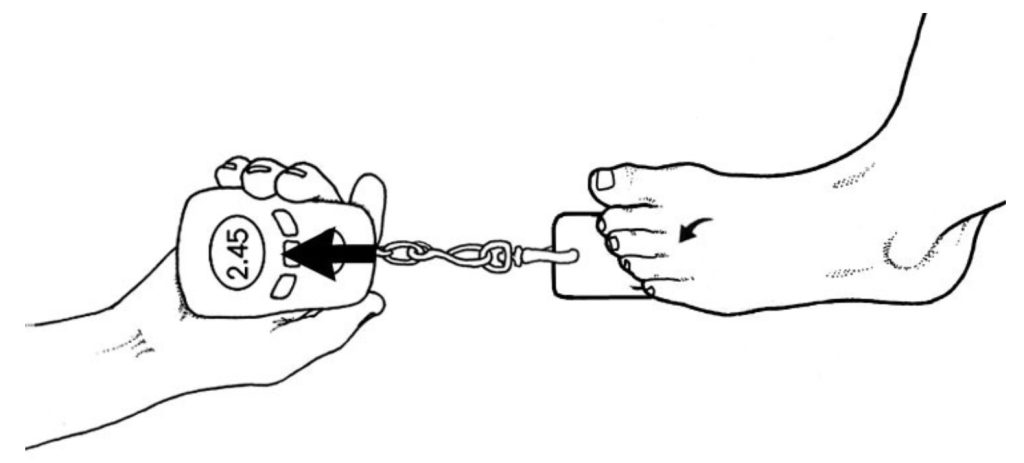
It is especially important that the patient focus on increasing pressure generated beneath the hallux while leaning forward and pushing back, as strength in the flexor hallucis longus is the single best predictor of falls in the elderly (3). In fact, Mickle et al. (6) show that for every 1% increase of body weight generated beneath the hallux, the risk of falling decreases by 7%. In other words, if a 100-pound female produces just 2 extra pounds of force beneath the big toe, her risk of falling decreases 14%. Note that the big toe alone can exert a downward force equaling 52% of body weight (7), and increasing force output by 1% is easy to achieve. In fact, it is common to have 30% increases in force generated beneath the hallux within a few months of performing this simple exercise. Once the patient masters the Vele Forward Lean, they can progress to more aggressive toe exercises, such as the AFX exerciser, or the ToePro foot/ankle exercise platform. In order to quantify strength gains with foot exercises, I recommend using a toe strength dynamometer (Fig. 2). This inexpensive device allows you to precisely measure toe strength beneath the hallux and lesser toes before and after exercise intervention. The initial strength scores provide the doctor and the patient clear proof of the need to perform toe exercises. The post-exercise scores also provide measurable guidelines for evaluating the efficacy of the exercise protocol. Because of the proven connection between toe weakness and falls in the elderly, evaluating and strengthening the toes should be a part of every senior’s daily exercise routine.
References:
- Petridou E, Manti E, Ntinapogias A, Negri E. What works better for community-dwelling older people at risk to fall? A meta-analysis of multifactorial versus physical exercise alone interventions. J Aging. Vol 21, Issue 5, 2009.
- Stubbs B, Brefka S, Denkinger M. What works to prevent falls in community-dwelling older adults? Umbrella review of meta-analyses of randomized controlled trials. Phys Ther. 2015;95:1095–1110.
- Mickle, K, et al., ISB Clinical Biomechanics Award 2009: Toe weakness and deformity increase the risk of falls in older people. Clinical Biomechanics. 2009;24:787-791.
- Endo M, Ashton-Miller J, Alexander N. Effects of age and gender on toe flexor muscle strength. Journals of Gerontology. Series A, Biologic Sciences Med Sciences. 2002. 57A(6):M392-397.
- Hill M, Duncan M, Oxford S, Price M. Effects of external loads on postural sway during quiet stance in adults aged 20-80 years. Applied Ergonomics. 2018; 66:64-69.
- Mickle K, Caputi P, Potter J, Steele J. Efficacy of a progressive resistance exercise program to increase toe flexor strength in older people. Clinical Biomechanics. December 2016;40:14-19.
- Jacob, H. Forces acting in the forefoot during normal gait: an estimate. Clinical Biomechanics. 2001;16:783- 792.