Every chiropractor knows that a strong, well-coordinated core is essential for maintaining spinal health. The core muscles work as a unit to increase intra-abdominal pressure providing just the right stiffness to unload the spine during lifting and loading tasks. Exercises such as side lying planks, bridges, bird-dogs, rollouts, and single-leg raises are prescribed to target the internal and external obliques, transverse abdominus, quadratus lumborum, and iliopsoas. Astute practitioners even recommend exercises for the pubococcygeus muscle, as weakness of the pelvic floor can impair core function.
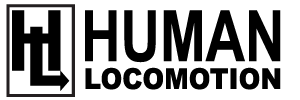
Unfortunately, none of the typically prescribed core exercises target the most active core muscle: the diaphragm (Fig. 1). In the course of a lifetime, the diaphragm, which is absent in birds and reptiles, contracts nearly 1 half-billion times, creating a negative pressure in the thorax that fills the lungs with air while maintaining a constant intra-abdominal pressure that provides stability to the spine when lifting and balancing (1).
The protective role the diaphragm has in preventing low back injuries is borne out in several studies. Animal research confirms electrically evoked diaphragm contractions enhance mechanical support of the spine (2). Human studies demonstrate that individuals with low back pain are more likely to present with smaller diaphragm excursions and higher diaphragm positions than asymptomatic individuals (3). The suboptimal diaphragm location forces the individual to increase their tidal volume during lifting in order to generate sufficient intra-abdominal pressure. Also, it has been proven that the diaphragms of individuals with low back pain fatigue more rapidly and to a greater extent compared to healthy controls (4). The important role the diaphragm plays in protecting the spine is supported by research showing that individuals with impaired pulmonary function, such as COPD, are much more likely to develop low back pain (5).
In an interesting EMG study of the diaphragm, Hodges and Gandevia (1) found the diaphragm is routinely activated during tasks that challenge stability of the spine, such as ballistic arm movements. These researchers note the diaphragm enhances stability by contracting before limb movements occur, and the intensity of diaphragmatic activation corresponds with the amplitude of forces perturbing the spine. The diaphragm serves the dual purpose of constantly working to control airflow for breathing, while also working with the transverse abdominus muscle to maintain a constant intra-abdominal pressure in order to stabilize the spine and protect against postural instability. Some research suggests the transverse abdominus, but not the internal/external oblique and/ or rectus abdominus muscles, have separate populations of motor units to control postural and respiratory functions (6).
The improved stability associated with proper diaphragm function is enhanced with subtle motions of the glottis. In a clever paper, Massery et al. (7) prove that because the degree of glottal opening regulates intra-abdominal and intrathoracic pressure, the glottal control of airflow plays an important role not only in maintaining intra-abdominal pressure, but also in maintaining balance. By inducing unanticipated shifts in standing subjects with different degrees of glottal opening, the authors note that subjects are able to more effectively balance when the glottis is only partially open. Unanticipated postural perturbations with either a fully closed glottis, as in a Valsalva maneuver, or a fully open glottis, as in actively sighing, cause the standing subjects to lose their balance more readily. This exaggerated shifting of the center of mass could be associated with an increased likelihood of falling with even minor postural perturbations. Improved stability with a partially open glottis explains why tennis players and other athletes often grunt while performing complex neuromotor tasks: the partially open glottis present while grunting may improve balance.
Perhaps the most interesting evaluations of diaphragm function comes from Belgium, where researchers prove that a weak diaphragm can impair core proprioception by decreasing sensitivity of spindles (Fig. 2) located in the erector spinae muscles (8). Apparently, because oxygen is necessary for our survival, the central nervous system prioritizes the delivery of blood to the diaphragm over other skeletal muscles. When the diaphragm fatigues
with exercise, the central nervous system deliberately decreases blood flow to spinal and peripheral muscles in order to shunt as much blood as possible to the diaphragm. If an individual’s diaphragm is weak, it prematurely fatigues and blood is redirected away from peripheral muscles to enhance diaphragmatic circulation. Several studies have shown significant reductions in blood flow to the erector spinae and lower extremity muscles when the diaphragm is deliberately exhausted (9,10). Where this gets interesting is the effect that decreased spinal and peripheral muscle circulation has on muscle spindles: because muscle spindles are highly vascular structures that exist almost exclusively in slow twitch muscle fibers (11), even a slight reduction of blood flow to a spindle, as would occur with premature fatigue of the diaphragm causing a reflex reduction in blood flow to the erector spinae, would markedly impair muscle coordination in the spine and extremity muscles. Impaired coordination of the spinal stabilizers is significant because it is correlated with the development of low back injury (12).
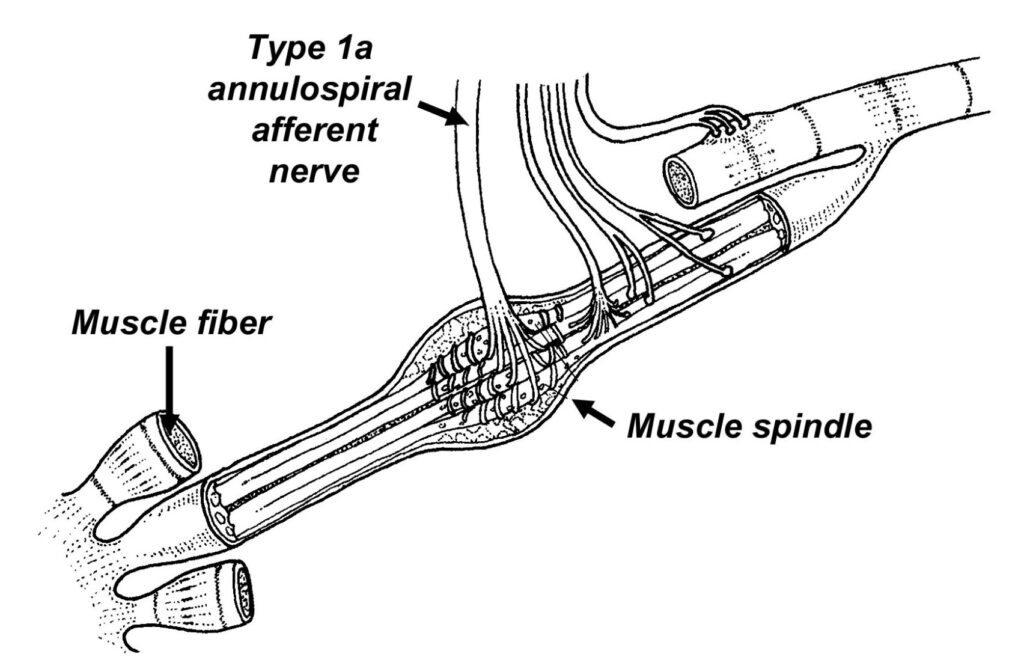
To prove diaphragm fatigue reduces low back proprioception, a team of researchers designed a fascinating study in which they placed small oscillating motors on soleus muscles as patients balanced with closed eyes. Because muscle vibration at 60 cps with 0.5 mm displacement stimulates the muscle spindle Ia afferents (13), these specially designed vibrating motors give the test subject the illusion the specific muscle being vibrated is lengthening. When an individual has faulty core proprioception, stimulation of the soleus muscle with vibration gives the subjects a sense that their calf muscles are lengthening and they immediately shift their body weight back in order to protect against falling forward. If the muscle spindles in their low back were working properly, the core muscles would sense that the soleus muscles were not actually lengthening and it was just an illusion (see supple- mental video). Using muscle vibration, researchers can identify whether individuals are incorporating multi-segmental proprioceptive control, in which both core and ankle proprioceptors are used equally, or an ankle-steered control, in which core proprioception is impaired and subjects rely more heavily on ankle proprioceptors.
Janssens et al. (9) prove the diaphragm can redirect blood flow from the erector spinae thereby reducing core proprioception by evaluating back muscle oxygenation using near-infrared spectroscopy before and after fatiguing the diaphragm in individuals with multi-segmental proprioceptive control and ankle-steered proprioceptive control (as determined with the vibrating motors). Their detailed evaluation confirmed that individuals who are over-reliant on ankle proprioceptors had significant reductions in back muscle oxygenation and blood volume with inspiratory fatigue. In contrast, individuals with multi-segmental proprioceptive control had no reduction in back muscle oxygenation when their muscles of inspiration were exhausted. These authors claim a fatigued diaphragm steals blood from the spinal stabilizers, decreasing reliance on core proprioceptors, greatly increasing the risk of injury. This research is significant as it explains why individuals using ankle-steered proprioceptive strategies are more likely to develop low back pain (14).
To see if the impaired core proprioception could be reversed with diaphragm exercises, Janssens et al. (15) per- formed another study in which they had individuals with low back pain undergo inspiratory muscle training. The test subjects performed 3 sets of 20 repetitions at either 60% full effort (high intensity group) or 20% full effort (low intensity group). After 8 weeks of training, individuals treated with the high intensity training exhibited smaller responses to ankle muscle vibration, improved core proprioception, higher inspiratory muscle strength, and most importantly, reduced low back pain severity. The authors note that these changes were not seen after low intensity inspiratory muscle training.
While the typical clinician does not have access to vibrating motors and force platforms, a simple way to evaluate core proprioception is to have the patient stand barefooted on a foam pad, such as the AirEx Balance Pad. Because the soft foam makes it difficult to rely on ankle proprioceptors, the standing patient is forced to rely on back muscle spindles, which when intact, allow the patient to balance with eyes closed while standing on foam with minimal sway. Exaggerated amounts of sway, which can exceed 3 or 4 inches in the sagittal plane, are common with impaired core proprioception. The impaired spinal proprioception is readily corrected with an 8-week training protocol that takes just a few minutes a day. From personal experience, the improved function associated with diaphragmatic breathing exercises occur more rapidly when done in conjunction with joint and soft tissue mobilization, both of which have been theorized to improve spinal proprioception.
References:
- Hodges PW, Gandevia SC. Changes in intra-abdominal pressure during postural and respiratory activation of the human diaphragm. J Appl Physiol. 2000;89(3):967–76.
- Hodges P, Kaigle Holm A, Holm S, Ekstrom L, Cresswell A, Hansson T, Thorstensson A. Intervertebral stiffness of the spine is increased by evoked contraction of transversus abdominis and the diaphragm: in vivo porcine studies. Spine. 2003;28:2594–2601.
- Kolar P, Sulc J, Kyncl M, et al. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012;42(4):352–62.
- Janssens L, Brumagne S, McConnell AK, Hermans G, Troosters T, Gayan-Ramirez G. Greater diaphragm fatigability in patients with recurrent low back pain. Respir Physiol Neurobiol. 2013;188(2):119–23.
- Janssens L, Brumagne S, McConnell AK, Hermans G, Troosters T, Gayan-Ramirez G. Greater diaphragm fatigability in patients with recurrent low back pain. Respir Physiol Neurobiol. 2013;188(2):119–23.
- Puckree T, Cerny F, and Bishop B. Abdominal motor unit activity during respiratory and nonrespiratory tasks. J Appl Physiol. 1998;84:1707–1715.
- Massery M, Hagins M, Stafford R, Moerchen V, Hodges PW. Effect of airway control by glottal structures on postural stability. J Appl Physiol. 2013;115(4):483–90.
- Janssens L, Pijnenburg M, Claeys K, McConnell AK, Troosters T, Brumagne S. Postural strategy and back muscle oxygenation during inspiratory muscle loading. Med Sci Sport Exerc. 2013;45(7):1355–62.
- Harms CA, Babcock MA, McClaran SR, et al. Respiratory muscle work compromises leg blood flow during maximal exercise. J Appl Physiol. 1997;82:1573-1583.
- Borghi-Silva A, Oliveira C, Carrascosa C, et al. A respiratory muscle unloading improves leg muscle oxygen- ation during exercise in patients with COPD. Thorax. 2008;63:910–915.
- Kokkorogiannis T. Somatic and intramuscular distribution of muscle spindles and their relation to muscular angiotypes. J Theoretical Biology. 2004;229(2):263–280.
- Claeys, K., Brumagne, S., Dankaerts, W. et al. Decreased variability in postural control strategies in young people with non-specific low back pain is associated with altered proprioceptive reweighting. Eur J Appl Physiol. 2011:111:115-123.
- Cordo PJ, Gurfinkel VS, Brumagne S, Flores-Vieira C. Effect of slow, small movement on the vibration-evoked kinesthetic illusion. Exp Brain Res. 2005;167(3):324–34.
- Claeys K et al. Young individuals with a more ankle-steered proprioceptive control strategy may develop mild nonspecific low back pain. J Electromyogr Kinesiol. 2015;25(2):329–338
- Janssens, L., McConnell, A. K. , Pijnenburg, M., Claeys, K., Goossens, N., Lysens, R., Troosters, T. and Brumagne, S., 2015. Inspiratory muscle training affects proprioceptive use and low back pain. Med Sci Sports Exerc. 2014;47(1), 12 -19.