In any given year, more than one in five runners will sustain a stress fracture (1). In the U.S. alone, this trans- lates into nearly 2 million stress fractures annually (2). In a study of 320 patients presenting with stress fractures, Matheson, et al., (3) note that 4 percent of these patients incurred the injury while playing basketball, 5 percent while playing tennis, 8 percent while in aerobics class, and a surprising 69 percent while running.
The running athlete is particularly prone to stress fractures, partly because of the repetitiveness of the activity and partly because running, unlike walking, has an airborne phase during which neither foot contacts the ground. Mann4 dramatizes this point by noting that a 150-pound man, when walking with a stride length of 2 1⁄2 feet for a distance of 1 mile, applies a force of 127 tons to his feet. If the same man were to run 1 mile, his stride length would increase to 4 1⁄2 feet and a force of 220 tons would be applied to his feet. When you consider the forces that must be dissipated over the course of a marathon (a long-distance runner’s feet contact the ground 5,000 times per hour, absorbing between one and three times body-weight), (3,4) it is no wonder that stress fractures are so prevalent in the running community.
Although it is generally accepted that the frequency and intensity of impact forces play a primary role in the development of stress fractures (these forces produce microdamage that exceeds the bone’s ability to remodel), they are by no means the sole cause. This was demonstrated in the study by Matheson, et al. (3), in that they could find no correlation between weekly mileage and the incidence of stress fracture. Also, only one in five of the stress fractures reported could be related to a sudden increase in impact forces, i.e., changing to a hard surface and/or a sudden increase in mileage.
Though rarely considered, muscle strength plays an important role in the prevention of stress fractures. In an interesting study of muscle volume and the development of stress fractures, Burne, et al. (5), determined that a 10-mm reduction in calf circumference resulted in a fourfold increase in the incidence of tibial stress fracture. This is consistent with research demonstrating lower extremity muscles prevent tibial fractures by adjusting to bony vibrations by pretensing prior to heel strike (6,7).
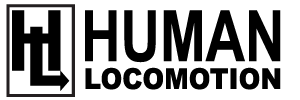
In addition to dampening the potentially dangerous bony oscillations following heel strike, certain muscles play a key role in creating compressive forces that allow various bones to resist bending strains present during the gait cycle. For example, the piriformis muscle, often considered to be unimportant during the gait cycle, has been shown to create a long-axis compression of the femoral neck that prevents it from bending with the application of vertical forces (Figure 1). Without adequate support from the piriformis and the synergistic lower gluteus medius, a bending force would be created in the femoral neck capable of producing a fracture (a tension fracture on the superior side or a compressive fracture on the inferior side).
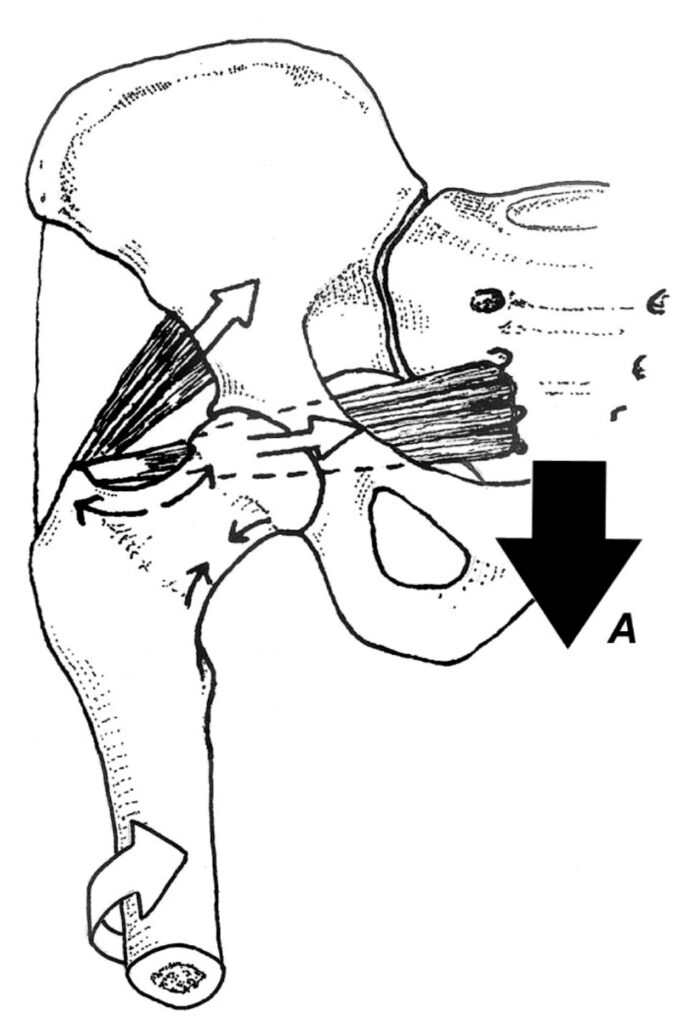
The ability of the piriformis to compress and stabilize the femoral neck is supported by the clinical observation that unlike most long bones exposed to significant bending forces, the femoral neck possesses only a thin layer of cortical bone that, without muscular reinforcement, would be unable to resist the bending forces present during propulsion. Specific exercises to strengthen the piriformis and gluteus medius are illustrated in Figure 2.
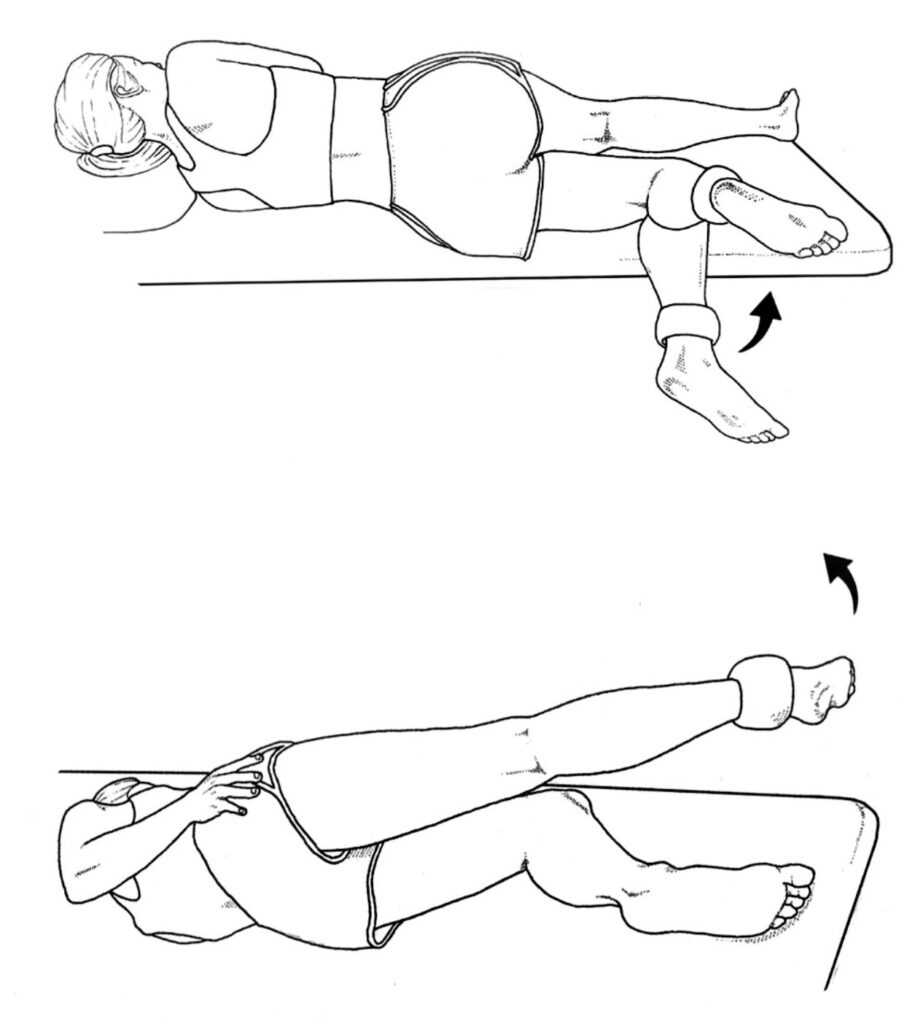
While the piriformis has been proven to protect the femoral neck, the iliotibial band has recently been shown to create a stabilizing force along the entire thigh that lessens bending of the femur during the midstance period of the gait cycle. Contrary to most published literature, Falvey, et al. (8), discovered the iliotibial band possesses a fibrous slip along its entire length that attaches to the posterior aspect of the femur along the linea aspera. The researchers also discovered the ITB has a tendon-like insertion along the lateral aspect of the distal femur that serves as a powerful fibrous anchor (Figure 3).
During the midstance phase of the gait cycle, contraction of the tensor fascia latae and gluteus maximus muscles creates a compressive force that is transmitted through the length of the entire femur, preventing it from bending with the application of ground-reactive forces during midstance. As a result, the treatment of femoral shaft stress fractures should include strengthening exercises for the tensor fascia latae and gluteus maximus muscles. The lateral compressive force created by the ITB explains why individuals with medial knee arthritis have reduced rates of arthritis progression when their hip abductors are strong (9).
In an interesting paper evaluating the bending forces present in the metatarsal shafts during the propulsive period, Ferris, et al. (10), embedded strain gauges in the metatarsal shafts of cadaveric feet and evaluated bending forces present during simulated propulsion as the long digital flexor muscles were either tractioned or relaxed with pneumatic actuators (Figure 4). Using this elaborate technique, the researchers determined that when the digital flexor muscles were relaxed, significant bending strains were present in the metatarsal shafts, which in real life would have created a bending force capable of fracturing bone. When the muscles were tractioned, they created a powerful compressive force along the plantar metatarsal shafts that greatly reduced bending strains. The authors speculate that strengthening the digital flexors “may play a role in the prevention of metatarsal stress fractures.” I’ve used the exercise illustrated in Figure 5 to treat recurrent metatarsal stress fractures with excellent results.
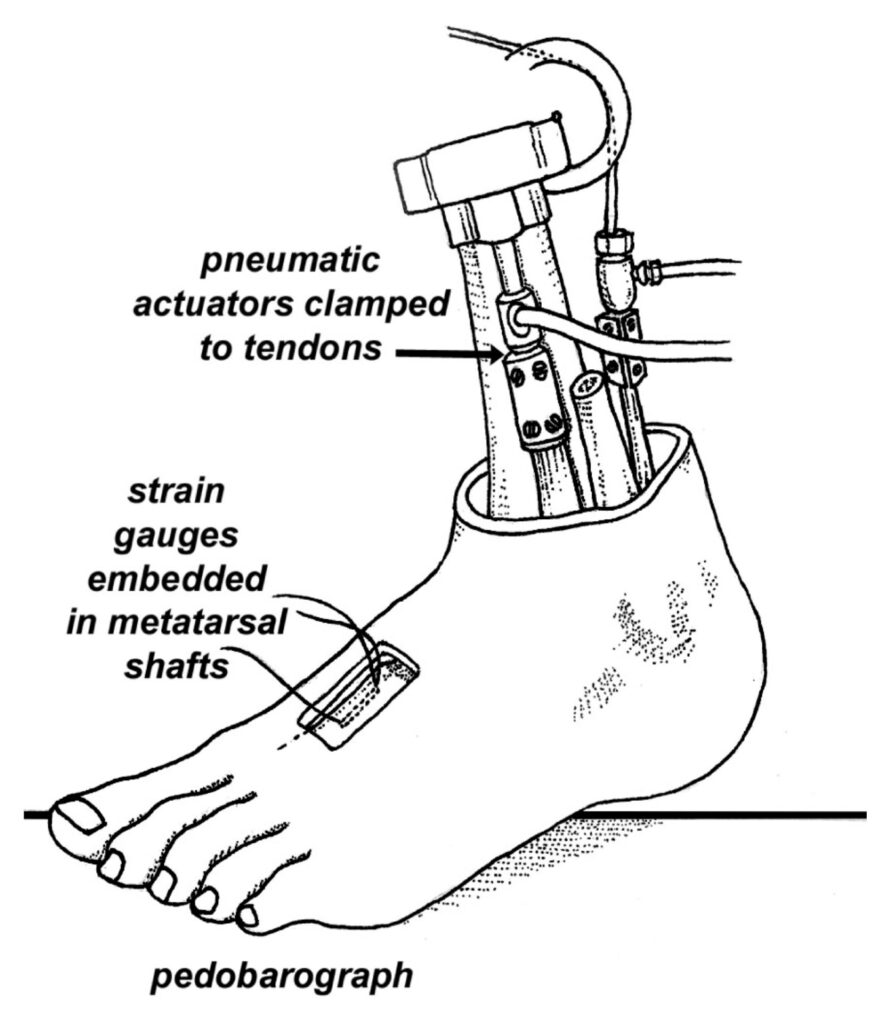
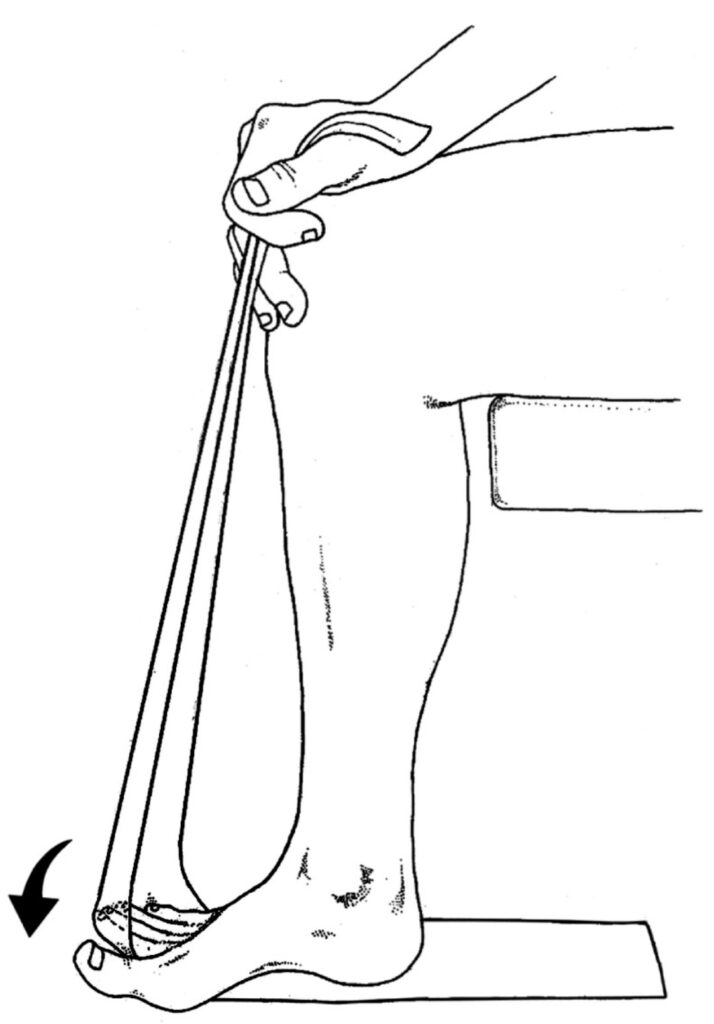
Fig. 5. Flexor digitorum longus home exercise. The seated patient places a Thera-Band® beneath the foot, traversing beneath the lesser toes up to the knee. Tension in the band is determined by the pulling force at the knee and the patient actively plantarflexes the toes against resistance (arrow). To strengthen flexor hallucis longus, this exercise is repeated beneath the big toe. Eight sets of 40 repetitions are usually performed daily.
While most clinicians believe stress fractures result from a defect in the inherent strength of the bone itself, a common, yet frequently overlooked cause of stress fracture is the inability of the muscular stabilizing system to lessen bony vibration and prevent bending in an otherwise healthy bone. In many cases, the addition of a few simple strengthening exercises may accelerate recovery and lessen the potential for reinjury.
References:
- Bennell K, Malcolm S, Thomas S, et al. The incidence and distribution of stress fractures in competitive track and field athletes. A twelve-month prospective study. Am J Sports Med, 1996;24:211-217.
- Crowell H, Milner C, Hamill J, Davis I. Reducing impact loading during running with the use of real-time visual feedback. J Orthop Sports Phys Ther, 2010;40:206
- Matheson GO, Clement DB, McKenzie DC. Stress fractures in athletes. A study of 320 cases. Am J Sports Med, 1987;15:46-58.
- Mann R. Biomechanics of Running, In: Mack (ed). Symposium of the Foot and Leg in Running Sports. St. Louis: CV Mosby, 1982;1-29.
- Burne S, Khan K, Boudville P, et al. Risk factors associated with exertional medial tibial pain: a 12-month prospective clinical study. Br J Sports Med, 2004;38:441-445.
- Wakeling J, Nigg B. Modifications of soft tissue vibrations in the leg by muscular activity. J Appl Physiol, 2001;90:412-420.
- Wakeling J, Liphardt A, Nigg B. Muscle activity reduces soft-tissue resonance at heel-strike during walking. J Biomech, 2003;36:1761-1769.
- Falvey E, Clark R, Franklyn-Miller A, et al. Iliotibial band syndrome: an examination of the evidence behind a number of treatment options. Scand J Med Sports, 2010;20:580-587.
- Chang A, Hayes K, et al. Hip abduction moments and protection against medial tibiofemoral osteoarthritis progression. Arth Rheum, 2005;52:3515-3519.
- Ferris L, Sharkey N, Smith T, et al. Influence of extrinsic plantar flexors on forefoot loading during heel rise. Foot Ankle, 1995;16:464-473.