- Achilles injuries are common, and the most frequently prescribed exercise interventions have relatively poor long-term outcomes.
- New research shows heavy-resistance long-duration isometric contractions accelerate tendon repair by increasing the outflow of fluid from the center of the Achilles tendon.
- The gliding of neighboring individual fibers of the Achilles tendon against one another also stimulates tendon remodeling, and this is best accomplished with bent knee heel raises.
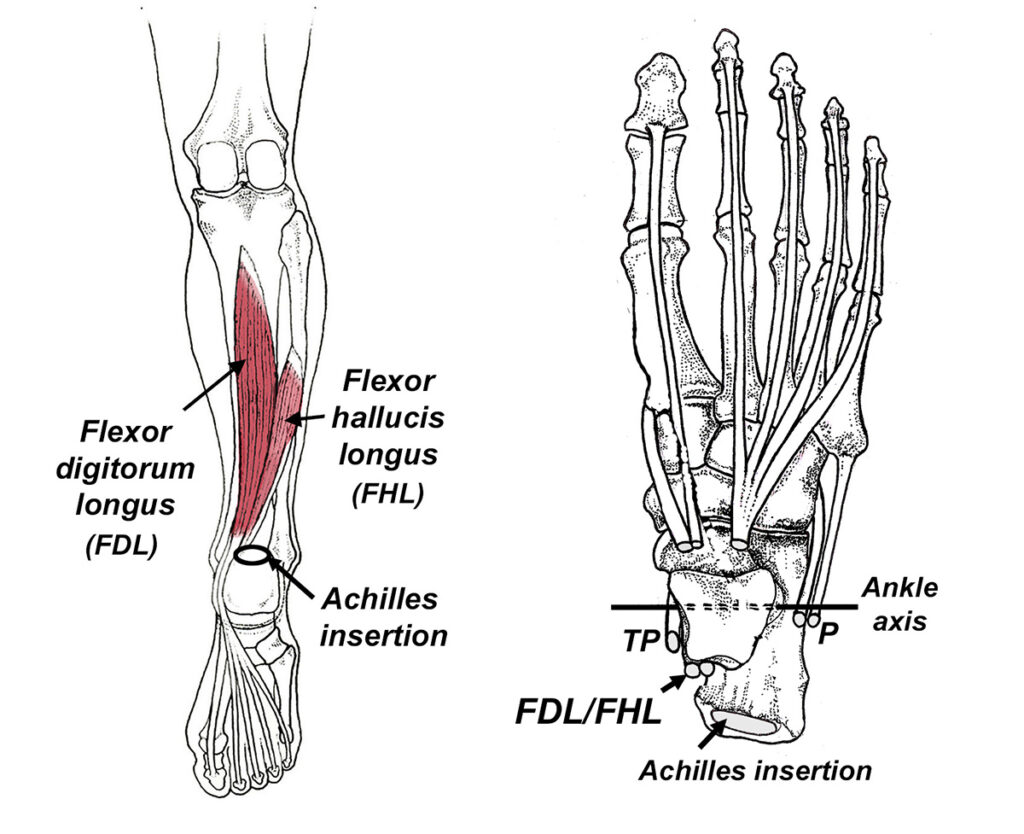
- For best outcomes, it is important to reduce stress on the Achilles tendon by strengthening its synergists. Flexor hallucis longus is particularly effective at offloading the Achilles tendon.
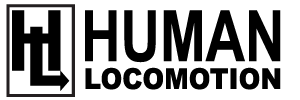
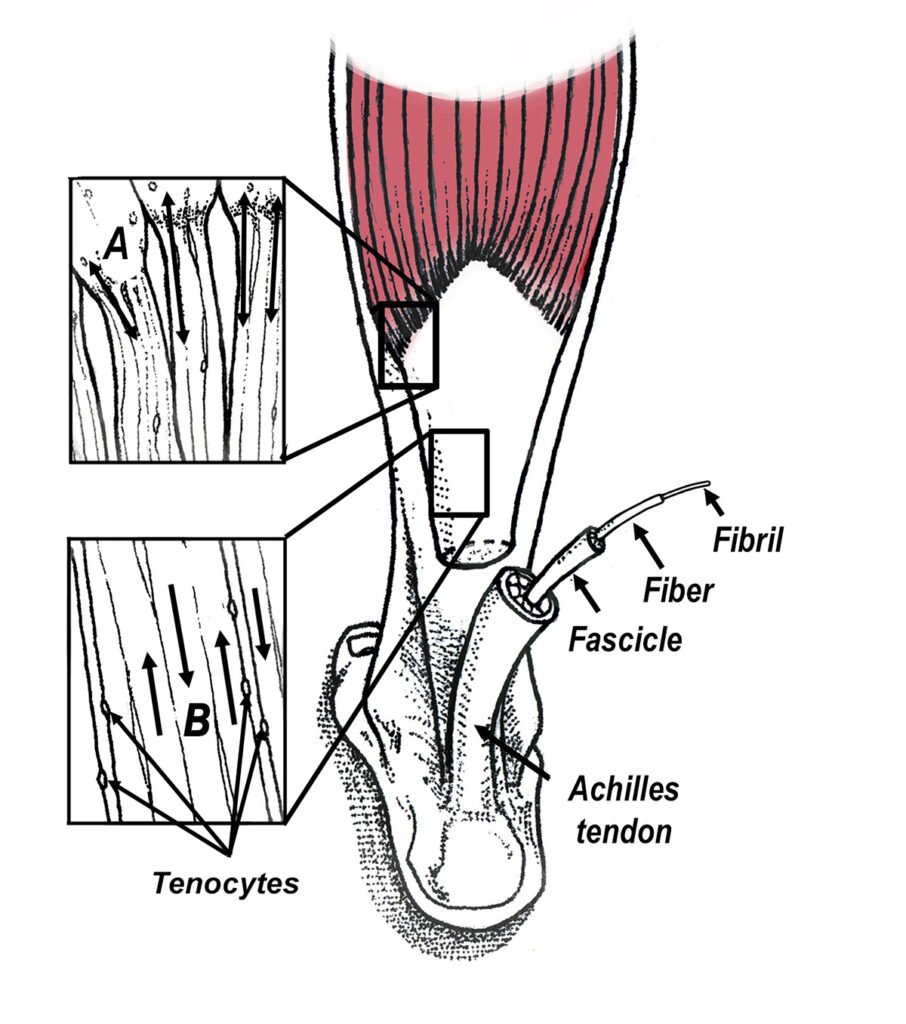
The Achilles tendon is a remarkable structure that has the ability to store and return nearly 90% of the energy it takes to stretch it (1). Because different fibers of the Achilles tendon rotate between 26° and 136° before attaching to the calcaneus (2), they function like coiled springs, absorbing and returning 10 times more energy than the neighboring gastrocnemius and soleus muscles (Fig. 1). The free energy supplied by this elastic recoil significantly reduces the metabolic cost of locomotion and has played a huge role in our success as bipeds (3). Unfortunately, despite its size and significant strength, the Achilles tendon is injured with surprising regularity, especially in running athletes. In any given year, nearly 10% of runners develop Achilles tendinopathy, and the lifetime prevalence of Achilles injuries in middle and long distance runners is nearly 50% (4). Although occasionally injured at the insertion point on the calcaneus, the vast majority of Achilles injuries occur at the midportion of the Achilles tendon and are referred to as non-insertional tendinopathies. The higher frequency of non-insertional injuries is the result of the naturally impaired circulation present in the midsection of the Achilles tendon. While the limited number of blood vessels allows the midsection to tolerate extremely high forces, it also results in impaired cellular remodeling following trauma.
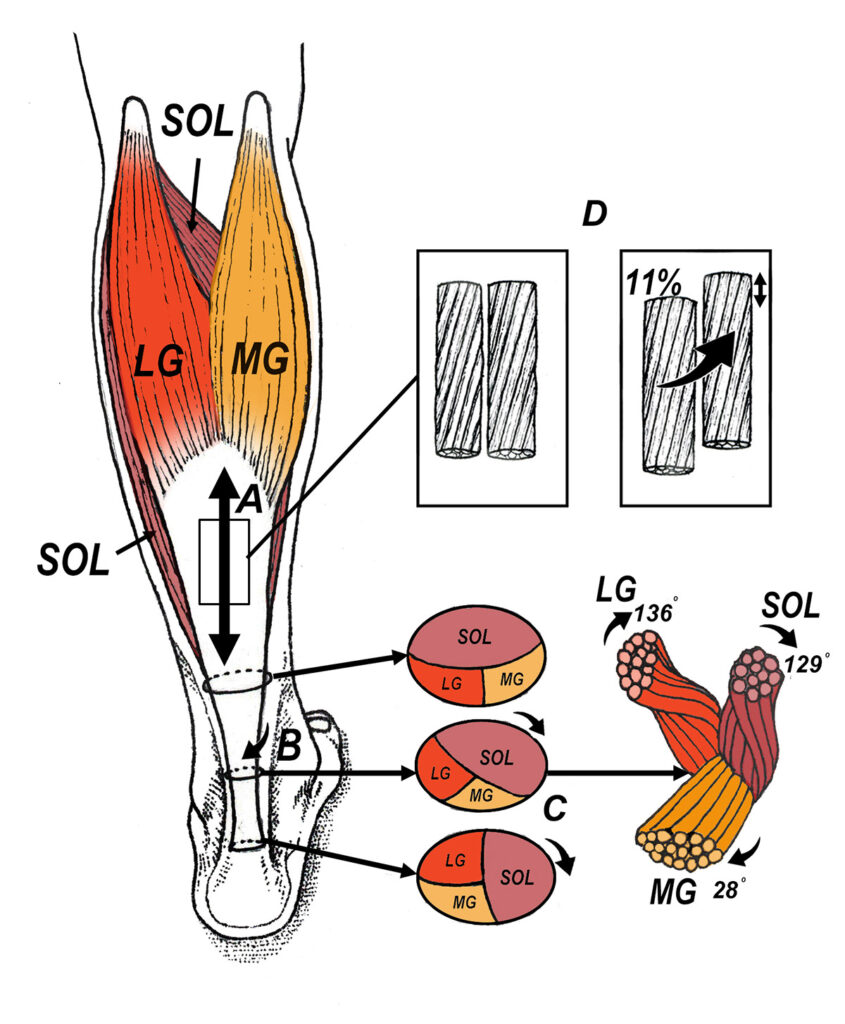
Fig. 1. As the Achilles tendon lengthens while walking and running (A), fibers from the corresponding muscles rotate 90° (B and C), and neighboring fibers in the Achilles tendon can separate by more than 11% (D). The combination of tendon fiber twisting and sliding allows the Achilles tendon to store and return 10 times more energy than the gastroc and soleus muscles and twice as much energy as the arch (25). Notice how tendon fibers originating from the lateral gastrocnemius and soleus muscles rotate significantly more than fibers from the medial gastrocnemius. The greater degree of tendon twisting in the lateral gastroc and soleus makes these muscles more important with storing and returning energy, while the medial gastroc plays a significant role in rapid force production, explaining the high prevalence of tears in the medial gastroc with jumping sports. Abbreviations: LG: lateral gastrocnemius; MG: medial gastrocnemius; SOL: soleus.
Far and away the most popular exercise prescription for managing non-insertional Achilles injuries is the eccentric training protocol originally described by Alfredsson et al. (5) more than 25 years ago. This routine consists of having the patient perform 3 sets of 15 repetitions of both straight and bent knee exercises twice daily (Fig. 2). Patients are told to exercise through discomfort, and the exercises are done 7 days per week. Unfortunately, despite its widespread use for almost 3 decades, the Alfredson protocol has been proven to be only moderately effective at reducing long-term symptoms associated with Achilles tendinopathy, as nearly 60% of people treated with this intervention report pain and continued discomfort 5 years later (6).
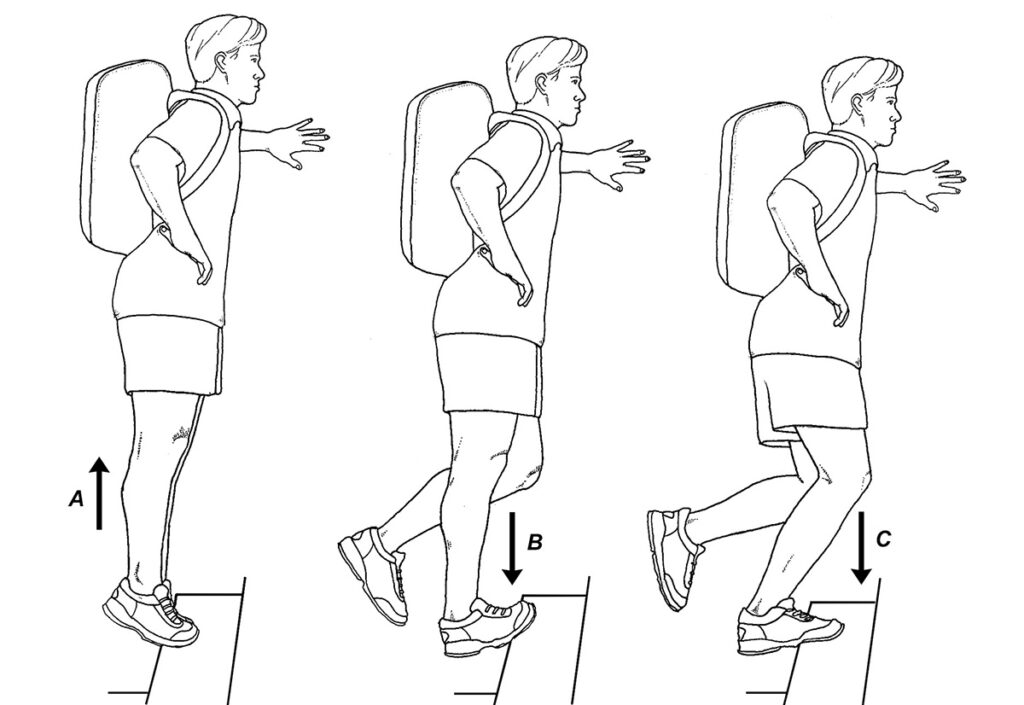
In an attempt to improve outcomes associated with exercise therapy, researchers have realized that it is important to understand the exact mechanism in which exercise stimulates recovery. To that end, some interesting new research out of Australia shows that fluid flow dynamics within the Achilles tendon may play a key role in accelerating recovery (9). These authors cite numerous studies showing when a healthy tendon is exercised, there is a significant flow of fluid away from the core of the tendon, and the shear stress from this fluid flow creates a tensile strain that stimulates tenocyte remodeling (10-12) (Fig. 3). This outflow of fluid is absent in tendinopathic tendons. To identify which exercises most effectively stimulate intratendinous fluid flow, the authors used 3-dimensional ultrasonography to monitor flow dynamics as participants performed isometric contractions at intensities that varied from 35 to 75% full effort, with load durations ranging from 2 to 8 seconds. Upon completion of the study, the authors determined the subjects performing the heavy-load, long-duration exercises had a 13% reduction in tendon volume, which was far and away greater than any other treatment group. As a result, the authors state that in order to accelerate tendon repair, “the applied load must be heavy and sustained for long-duration.”
In perhaps the most interesting recent research on the underlying causes of Achilles tendinopathy, researchers from Finland show that when people with healthy Achilles tendons exercise, different portions of the gastrocnemius and soleus muscles pull on their corresponding tendon fibers, creating a nonuniform pattern of interfascicular sliding within the Achilles tendon (13). The nonuniform sliding of one tendon fiber against another mechanically stimulates tenocytes to accelerate tendon remodeling (Fig. 4). In contrast to healthy tendons, individuals with damaged Achilles tendons show a more uniform pattern with limited variation in interfascicular sliding. The clinical significance of this paper is huge, as it confirms that in order for the Achilles tendon to be effectively rehabilitated, all fibers of the different calf muscles must participate in force generation, as activity in each muscle gets transferred into the tendon promoting the nonuniform pattern of fascicle sliding present in healthy tendons.
To identify exactly which exercises increase the amount of interfascicular sliding, Handsfield et al. (14) evaluated tendon fiber sliding patterns as people performed different calf exercises. Of all the exercises studied, the bent knee heel drop exercise that specifically targets the soleus muscle produced the greatest increase in interfascicular sliding while simultaneously placing the least stress on the tendon. The authors claim that this exercise will have “a major role in the future of tendon rehabilitation.” The outcome of this paper is consistent with recent research showing that weakness of the soleus is the single best predictor of non-insertional Achilles injury (24). Because the soleus possesses 50% more muscle mass than the neighboring gastrocnemius muscles, failure of the soleus to generate force would significantly impair interfascicular tendon sliding, which could be corrected with bent knee heel drop exercises.
To be consistent with the latest research, the ideal exercise prescription for managing Achilles injuries should include bent knee heel drops to enhance intratendinous fascicle sliding, and heavy-load long-duration isometric contractions to increase fluid outflow from the tendon. I typically recommend 4 sets of 24 repetitions of the exercises illustrated in figure 5, as the 4×24 protocol produces the same increase in muscle volume as heavy-load resistance training (15). Notice that at the end of each set, a 30-second isometric contraction is performed to enhance the outflow of fluid from the tendon. In my opinion, the isometric component of this exercise is the key to tendon recovery. In addition to improving fluid dynamics, Keith Baar (16) states that when a damaged tendon is forced to undergo a prolonged isometric contraction, the healthy fibers slowly slide over one another, exposing the stiffer damaged fibers to the mechanical stress necessary to remodel. Dr. Baar and others (17) measured the most important enzymes responsible for creating the cross-links associated with tendon repair, such as lysal oxidase and ERK1/2, and showed that after the first 10 minutes of isometric contractions, the levels of these important enzymes dropped significantly and became inactive for a full 6 hours. The clinical implication of this research is that the isometric components of these exercises can be performed twice per day, at 6 hour intervals. In contrast, the strengthening component should be performed just once a day.
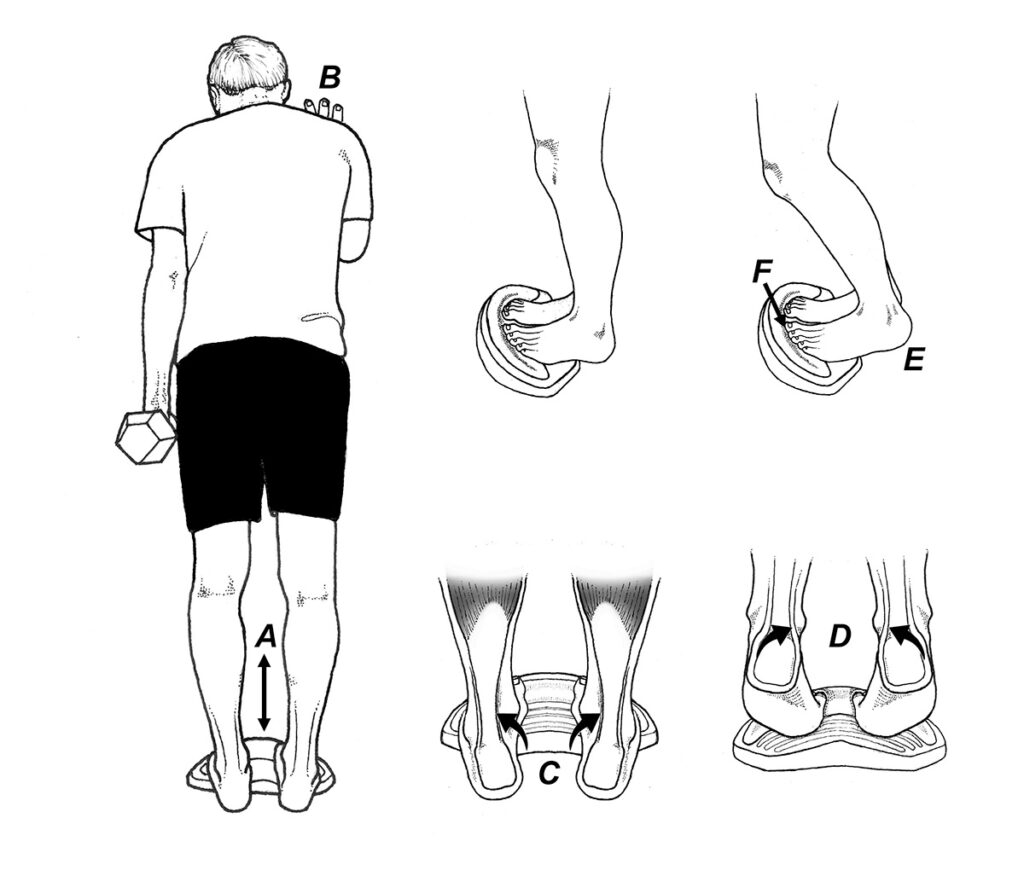
Fig. 5. Home exercise protocol for non-insertional Achilles injuries. Place the ToePro next to a wall andperform 4 sets of 24 repetitions going through a full range of motion ( A ). You should perform 2 sets with your kneesstraight and 2 sets with knees bent. You should contact the wall to maintain balance ( B ) and if necessary, hold ontoa weight to ensure that you’re fatigued by the 24th repetition. If you are unable to do 24 repetitions, perform theexercise next to a table so you can push down with your hands to offload your calves. While doing this exerciseroutine, you should move your feet from full inversion to full eversion ( C-D ) and after completing each set, youshould perform a 30-second isometric contraction with your heels position just slightly off the floor ( E ). If you areextremely strong, you can do the isometric contraction on one leg at a time. To strengthen important synergists tothe Achilles tendon, make sure you push down vigorously with your toes while performing these exercises ( F ).
Although these exercises can be performed on a stairway or an angled foam platform, I typically have the patient perform the exercises while standing on a ToePro. The main advantage to using the ToePro is that it markedly increases activity of the flexor hallucis and flexor digitorum longus muscles, which have long lever arms to the ankle axis and are capable of significantly offloading the Achilles tendon during recovery (Fig. 6). By exercising the toe muscles in a lengthened position, strength gains are increased nearly fourfold compared to conventional exercises (18). It’s not just toe muscles that respond to exercising in lengthened positions. A growing body of research is showing that exercising all muscles in their lengthened positions accelerates muscle remodeling (19-21), and results in greater transference to dynamic performance (22).
I’ve been using this exercise protocol for almost 2 years now, and in my experience, it definitely produces better outcomes than the Alfredson protocol, especially in elite athletes. Although it requires a fair amount of commitment to perform these exercises daily, some recent research shows that even people who perform their Achilles exercise routine with reduced intensity and for a shorter period of time still get good outcomes (23). Because the ideal exercise frequency has yet to be determined, I base the frequency prescription on the individuals’ level of fitness: extremely fit people should perform these exercises daily, with the isometric contractions performed twice a day, and less fit and/or older individuals should perform them 3 times a week, with the isometric components performed just once a day. The reduced frequency definitely increases compliance, which also increases the probability of a successful long-term outcome.
References:
- Finni T, Vanwanseele B. Towards modern understanding of the Achilles tendon properties in human movement research. J Biomech. 2023;13:111583.
- Pekala P, et al. The twisted structure of the Achilles tendon unraveled: A detailed quantitative and qualitative anatomical investigation. Scand J Med Sci Sports. 2019:1842-1842
- Bramble D, Lieberman D., Endurance running and the evolution of Homo. Nature. 2004:345 – 352.
- Kujala U, et al. Cumulative incidence of Achilles tendon rupture and tendinopathy in male former elite athletes. Clin J Sport Med . 2005;15:133-5.
- Alfredson H , Pietilä T , Jonsson P , et al . Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998 ;26:360–6.
- van der Plas A, et al. A 5-year follow-up study of Alfredson’s heel-drop exercise programme in chronic midportion Achilles Tendinopathy. Br J Sports Med 2012: 46 :214–218.
- Malliaras P, et al. Achilles and Patellar Tendinopathy Loading Programmes. Sports Med. 2013;43:267–286.
- Funaro A, et al. Subject- Specific 3D Models to Investigate the Influence of Rehabilitation Exercises and the Twisted Structure on Achilles Tendon Strains. Front Bioeng Biotechnol. 2022; 10:914137.
- Merza E, et al. The acute effects of higher versus lower load duration and intensity on morphological and mechanical properties of the healthy Achilles tendon: a randomized crossover trial. J Exper Biology. 2022;May 15:225.
- Docking S, et al. Relationship between compressive loading and ECM changes in tendons. Muscles, Ligaments and Tendons Journal. 2013;3:7.
- Wall M, et al. Cell signaling in tenocytes: response to load and ligands in health and disease. Metabolic influences on risk for tendon disorders. 2016:79-95.
- Iwanuma S, et al. Longitudinal and transverse deformation of human Achilles tendon induced by isometric plantar flexion at different intensities. J Applied Phys. 2011;110:1615-21.
- Khair R, Stenroth L,et al. Non‐uniform displacement within ruptured Achilles tendon during isometric contraction. Scan J Med Sci Sports. 2021;31:1069-77.
- Handsfield G, et al. Achilles subtendon structure and behavior as evidenced from tendon imaging and computational modeling. Frontiers Sports and Active Living. 2020;23;2:70.
- Burd N, et al. Low-load high-volume resistance exercise stimulates muscle protein synthesis more than high-load low-volume resistance exercise in young men. PLoS ONE . 2010; 5(8):e12033.
- Baar K. Training to improve musculoskeletal performance and accelerate return to play. Keynote lecture at the Sports Congress in Copenhagen, 2018.
- Paxton J, Hagerty P, Andrick J, Baar K. Optimizing an intermittent stretch paradigm using ERK1/2 phosphorylation results in increased collagen synthesis in engineered ligaments. Tissue Engineering Part A. 2012 Feb 1;18:277-84.
- Goldmann J, et al. The potential of toe flexor muscles to enhance performance. J Sports Sciences. 2012;31:424-433.
- Kruse A,et al. Stimuli for Adaptations in Muscle Length and the Length Range of Active Force Exertion-A Narrative Review. Front. Physiol. 2021. 12:742034.
- Guex K, et al. Hamstring Architectural and Functional Adaptations Following Long vs. Short Muscle Length Eccentric Training. Front. Physiol. 2016;7:340.
- McMahon G, et al. Muscular adaptations and insulin‐like growth factor‐1 responses to resistance training are stretch‐mediated. Muscle & Nerve. 2014;49:108-19.
- Oranchuk D, et al. Isometric training and long‐term adaptations: Effects of muscle length, intensity, and intent: A systematic review. Scan J Med Sci Sports. 2019;29:484-503.
- Stevens M, Tan C. Effectiveness of the Alfredson protocol compared with a lower repetition-volume protocol for midportion Achilles tendinopathy: a randomized controlled trial. J Orthop Sports Phys Ther. 2014;44:59-67.
- O’Neill, S, Barry, S, Watson, P, Plantarflexor strength and endurance deficits associated with mid-portion Achilles tendinopathy: The role of soleus. Phys Ther Sports. 2019.
- Ker R, Bennett M, Bibby S, et al. The spring in the arch of the human foot. Nature. 1987;325:147-149.
- Wirth S, et al. Flexor hallucis longus hypertrophy secondary to Achilles tendon tendinopathy: an MRI‑based case–control study. Europ J of Orthop Surg Trauma. 2021; 31:1387–1393.