Excerpted from his book, Human Locomotion
Limb length discrepancy (LLD), which is divided into functional and structural categories, is a common cause of injury. In a study of 3,026 subjects with radiographically confirmed LLD, Harvey et al. (152) determined that individuals with 1 cm discrepancies are more likely to develop knee pain and osteoarthritis on the side of the short limb, while discrepancies of 2 cm or more are associated with the development of pain and osteoarthritis in both knees. Fortunately, most people present with lower extremities of relatively equal length. Although small discrepancies are common, limb length differences greater than 1 cm occur in less than 1 in 1,000 people (162). This contrasts with the upper extremities, where large length differences are common (341). Trivers et al. (341), attribute the smaller length disparities in the lower extremities to natural selection favoring equal limb lengths, since muscular compensation for large LLD is metabolically expensive.
Despite the higher prevalence of knee osteoarthritis on the side of the shorter limb, overall, the longer limb is more likely to be injured because it is exposed to greater ground-reactive forces and isometric torque (167). This is consistent with a study by Friberg et al. (153), who evaluated Norwegian military recruits and noted that 73% of stress fractures occurred in the long limb, 16% in the short limb, and 11% of stress fractures occurred in limbs of equal length. The long limb hip is also prone to injury. In a study of 100 patients presenting for total hip replacement, Tallroth et al. (154) determined that 84% had arthritis on the side of the long limb. Although injury is usually associated with discrepancies greater than 1.6 cm, discrepancies as small as 1 cm have been associated with development of low back pain (155,156) and plantar fasciitis (157). Additionally, functional limb length discrepancy secondary to asymmetrical pronation may be an etiological factor in the development of sciatica (158).
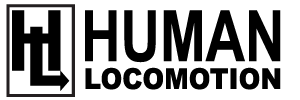
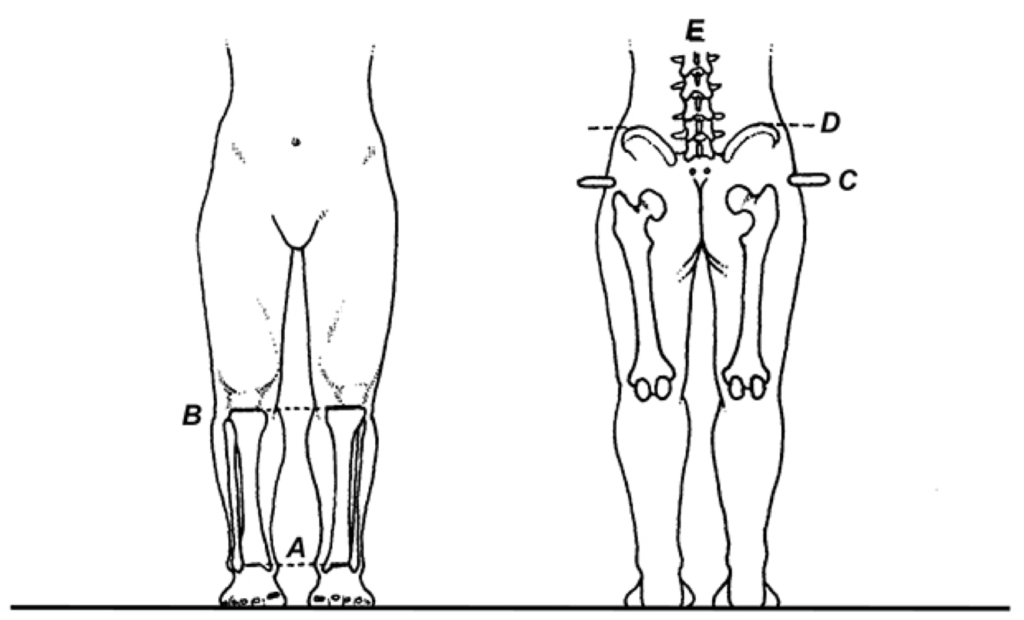
Because they are treated differently, it is important to differentiate a structural limb length discrepancy (which represents a fixed osseous malformation) from a functional limb length discrepancy (which is most often the result of asymmetrical pronation and/or soft tissue contracture in the pelvis/spine). Unfortunately, differentiating these two deformities is not always easy. In many cases, structural and functional limb length discrepancies occur together, one masking the actual degree of the other (Fig. 4.84).
A) A functional limb length discrepancy on the left, which is secondary to asymmetrical pronation (B), coupled with a structural limb length discrepancy of the right femur (C), gives the appearance of symmetrical limb lengths. In (D), the rigid plantarflexed first ray on the right (E) produces a functional long limb on that side, which hides the right short femur (F).
To help differentiate structural from functional limb length discrepancy, several examination techniques have been developed. The most accurate of these tests is the scanogram. This technique involves taking a series of x-rays with the central ray initially level with the femoral head, then with the tibial plateau, and finally with the ankle mortise. Information from these x-rays gives exact information regarding the length of the femurs and tibias. An alternate method of x-ray evaluation involves positioning the standing patient with the feet directly beneath the femoral condyles, with the talonavicular joint maintained in a neutral position (which should be maintained muscularly by the patient) and the anterior superior iliac spines (ASISs) equidistant from the buckey.
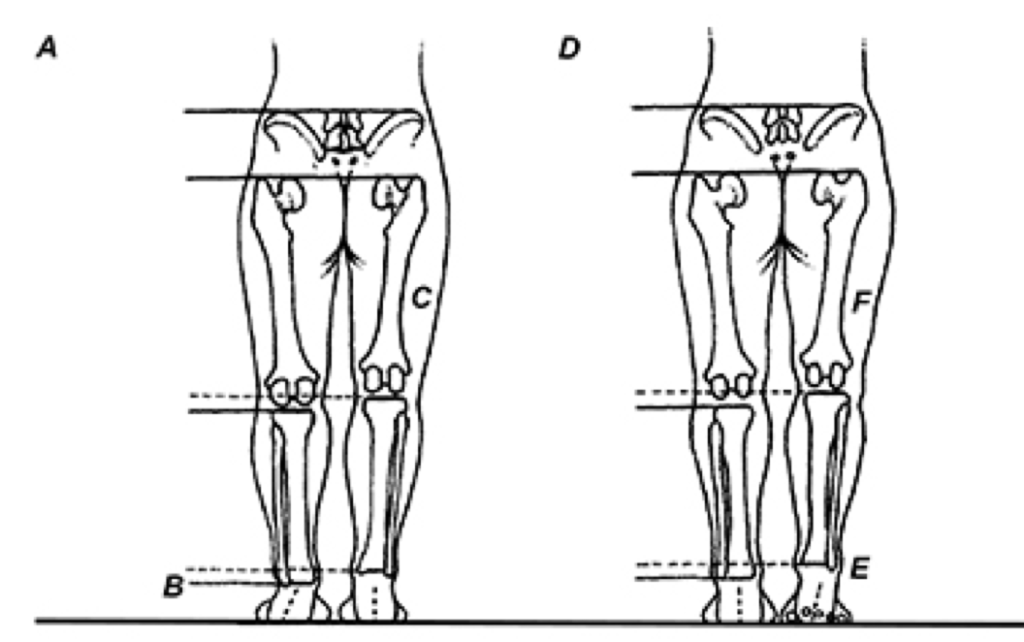
An x-ray taken with the central ray parallel to the femoral heads provides fairly accurate information regarding the relative lengths of the lower extremities (although it is unable to give exact information regarding lengths of the femurs and tibias). Regardless of which x-ray procedure is used to detect limb length discrepancy, the talonavicular joints should be maintained in their neutral positions, and the fem- oral neck angles should be measured and compared bilaterally, since these are common causes for functional and structural limb length discrepancies, respectively (Fig. 4.85).
If exposure to x-ray is a concern or if cost is prohibitive, structural limb length discrepancy may be identified with manual examination techniques. The most common method of evaluation is to position the patient supine and measure the distances from the ASIS to the medial malleolus. Unfortunately, asymmetrical muscle tension may tilt the pelvis, making it difficult to assess discrepancies less than 6 mm. To add to the problem, ASIS to medial malleolus measurements do not take into account the potential for limb length discrepancy arising from structural asymmetries distal to the medial malleolus; e.g., calcaneal fractures and unilateral collapse of the medial longitudinal arch.
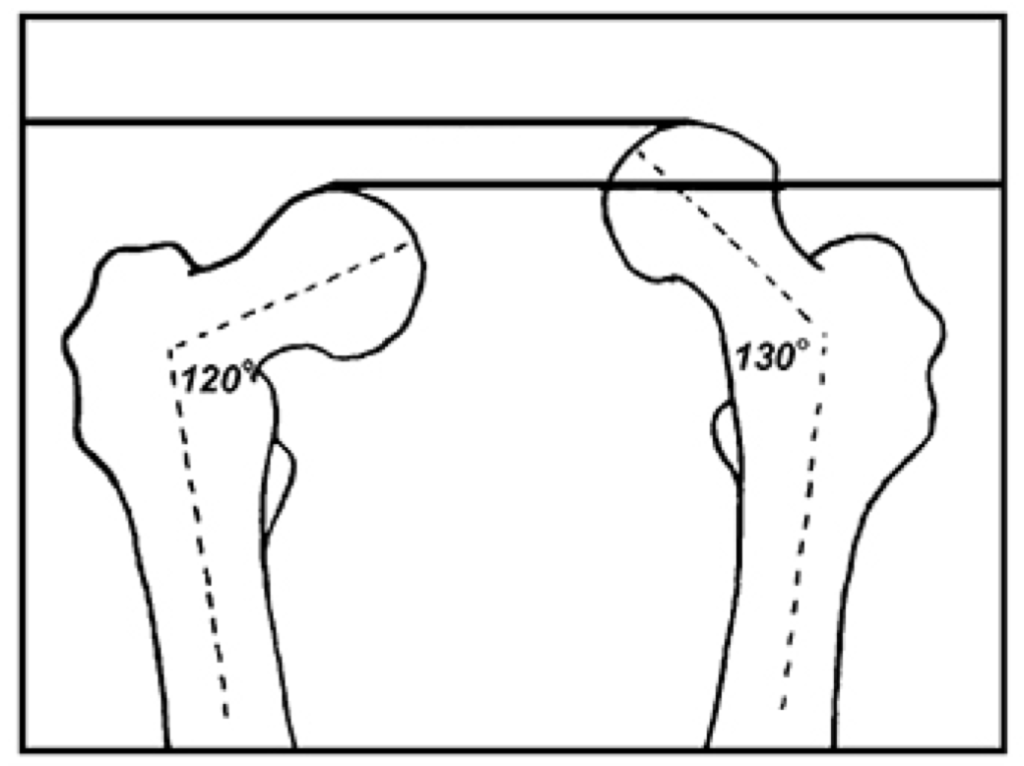
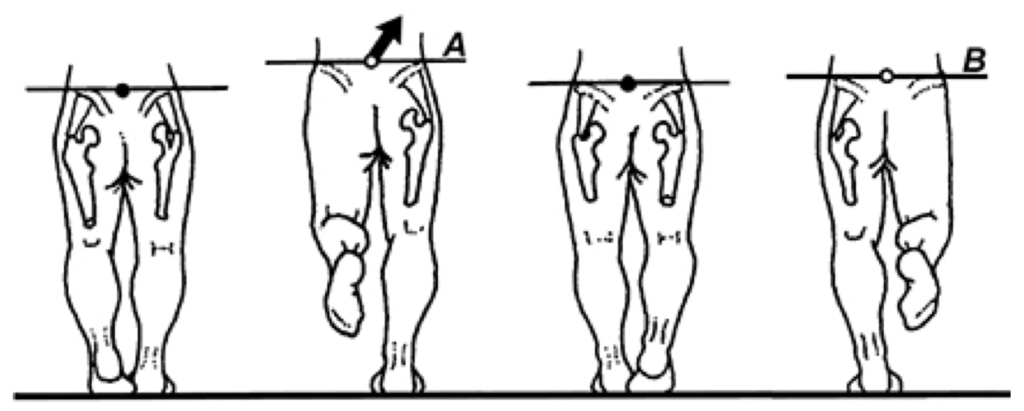
To be comprehensive, accurate evaluation of limb lengths often requires the examiner combine information from several different manual tests. To begin with, the relative lengths of the femurs and tibiae can be evaluated with Allis’ test (Fig. 4.86). Findings from this evaluation can then be compared to in- formation obtained from a weight-bearing evaluation, in which the levels of the various bony landmarks are observed from front and back (Fig. 4.87). As demonstrated by Hanada et al. (159), placing variable height shims beneath the shorter lower extremity until the iliac crests are level is a moderately valid and highly reliable method for determining the degree of even subtle limb length discrepancy. By combining information from the standing evaluation, with information from off weight-bearing and/or x-ray measurements, the practitioner is often able to differentiate structural from functional limb length discrepancy with moderate accuracy.
The examiner manually aligns the ASISs so that they rest on the same frontal and transverse plane (A). The medial malleoli are then placed together, and femoral lengths are evaluated from above (B), while tibial lengths are determined by com- paring the levels of the tibial plateaus (C).
The patient is carefully positioned with both feet directly beneath the greater trochanters. The level of the medial malleoli (A) can then be compared to determine whether asymmetrical subtalar pronation (or supination) is a cause of functional limb length discrepancy. Next, the tibial plateaus are compared (B) to determine the relative lengths of the tibiae. To compare femoral lengths, the fingertips are placed on top of the greater trochanters (which can be found by having the patient flex and extend the hips), and their respective levels are noted (C). Finally, the levels of the posterior superior iliac spine (PSISs) and iliac crests should be compared (D), and any deviation of the lumbar spine from vertical should be noted (E).
When present, an individual may compensate for a structural limb length discrepancy in a variety of ways. Because the short limb has a longer distance to fall during late swing phase, many individuals attempt to modify their gait by slowly lowering the shorter limb to the ground via eccentric contraction of
the contralateral hip abductor musculature. This frequently results in chronic strain of the gluteus medius muscle and may cause injury to the lumbar spine, since the lumbar vertebrae laterally flex towards the long limb. The effect of limb length discrepancy on spinal motion was demonstrated by Kakushima et al. (160), who noticed the addition of a unilateral 3 cm heel lift increased maximum lateral bending of the lumbar spine from 6.1° to 8.1°. The authors also noted that bending velocities were significantly larger when wearing the heel lift. The authors state the increased range and velocity of lumbar lateral flexion may eventually result in “disabling spinal disorders.” Although these effects were associated with the use of large heel lifts, limb length discrepancies as small as 9 mm have been correlated with the development of degenerative changes in the lumbar spine (162). In an attempt to stabilize against the increased lateral shear forces present at heel strike on the side of the short limb, some individuals develop a toe-out gait pattern prior to making ground contact. Although this protects against excessive lateral displacement of the center of mass, it increases the potential of a fibular stress fracture as toeout gait patterns have been shown to increase the transfer of forces through the fibula (163). This is consistent with Friberg’s study of military recruits demonstrating that although the long limb tibia is more prone to developing stress fracture, the fibula on the side of the short limb was more likely to fracture (153).
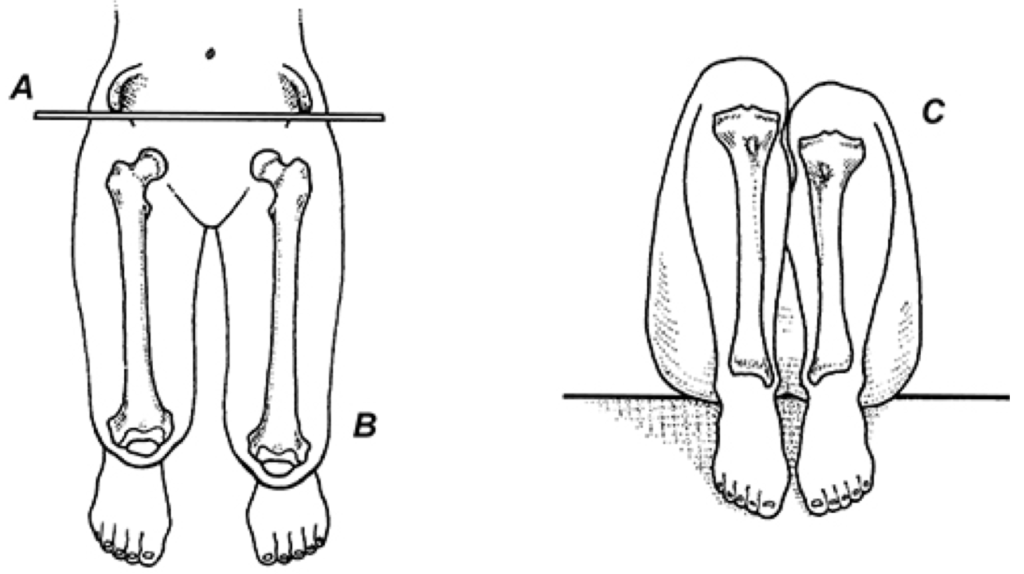
An alternate pattern of compensation for a short limb occurs when the individual hyperextends the knee and inverts the rearfoot on that side. While both of these motions may be helpful in bringing the heel closer to the ground during late swing phase, they may be damaging in that hyperextension of the knee impairs the quadriceps ability to dampen vertical forces, possibly explaining the higher prevalence of tibiofemoral osteoarthritis on the side of the short limb (152). The sacroiliac joint is also prone to injury on the side of the short limb as, in an attempt to level the pelvis, the innominate tilts anteriorly (164) (Fig. 4.88).
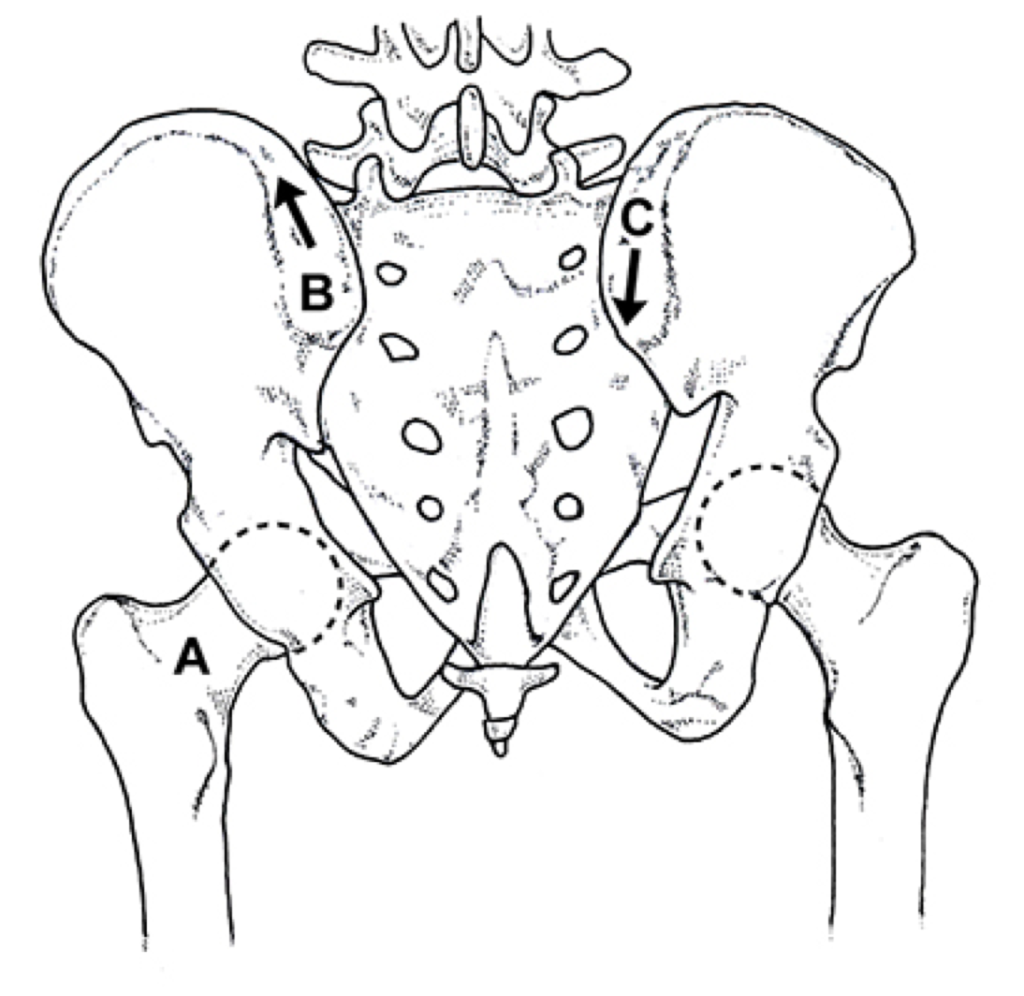
Because of the limited range of motion avail- able to this joint, the compensatory obliquity (which occurs as the pelvis twists between 2° and 6° [165]) greatly stresses the sacroiliac joint, possibly impairing its ability to absorb shock through sacral nutation because the ili- um is maintained in an end-range position. This may explain why the sacroiliac joint on the side of the short limb shows earlier and more exten- sive degenerative changes than the sacroiliac joint on the side of the long limb (166).
On the side of the longer lower extremity, in addition to increasing the potential for tibial stress fractures and osteoarthritis of the hip, compensation for a long limb may also produce injury at the foot and/or ankle. Because the long limb is subjected to greater pressure beneath the hallux, and the propulsive period on the side of the long limb occurs with a more rapid heel lift
(167), the potential for injuring the first metatarsophalangeal joint and/or the Achilles tendon greatly increases. Furthermore, because the long limb moves through a larger arc during swing phase (168), the individual often attempts to decrease the radius of this arc by flexing the knee, which may increase the potential for retropatellar injury during the contact period. While increasing the degree of knee flexion is the most effective way to compensate for a longer limb, it is also possible to bring the longer limb closer to the ground by maximally pronating the subtalar joint on that side.
Even though Sanner et al. (169) note an average vertical change of only 3 mm as the subtalar joint moves from a neutral position to a pronated position, it is possible for subtalar joint pronation to compensate for structural limb length discrepancies of 12 mm or more. In some cases, the head of the talus will actually make ground contact. Ironically, Hiss (170) claims that this makes the foot more stable, because plantar contact with the talar head serves as a point of support for the unstable medial column. As a result, even though it is a commonly held belief that the greater range of subtalar joint pronation occurs on the side of the structurally short limb, it is possible that an even greater range will occur on the side of the long limb if the individual attempts to level the pelvis.
Treatment in this situation requires placing a lift beneath the short limb and, if the range of subtalar joint pronation on the long limb side remains unchanged, an orthotic may be necessary to control the exaggerated motion. Novick and Kelley (171) note that the addition of a 2 mm thick functional orthotic produces a 4.8 mm elevation of the ankle joint’s center of mass secondary to superior repositioning of the talus on the calcaneus. Because of this, treatment for combinations of structural and functional discrepancies requires careful pre- and post-evaluation to ensure that proper correction has been attained. If a structural limb length discrepancy were present by itself, treatment should consist of placing the appropriately sized lift beneath the short limb.
The actual height of the lift is best determined by placing lifts of various sizes beneath the short limb and reevaluating alignment. The ideal lift will level the iliac crest and, more importantly, bring the lumbar spine to vertical (148). This technique is surprisingly accurate for even subtle limb length discrepancies. If a heel lift is recommended based upon information from off weight bearing measurements (e.g., ASIS to medial malleolus), it is necessary to add approximately 33% to the measured discrepancy in order to attain full correction; i.e., because the talus is positioned one third of the way between the calcaneus and metatarsal heads, a heel lift placed beneath the calcaneus will raise the talus only two thirds of that distance. For example, a 6 mm lift will raise the talus 4 mm. Because they may adversely alter motion and/or transfer weight to the medial forefoot, when possible, full length insole lifts are preferred over heel lifts.
Most authorities recommend that lifts be used for structural limb length discrepancies greater than 6 mm (172,173). However, Subotnick (174) claims that because of the 3-fold increase in ground-reactive forces associated with running, heel lifts should be used on running athletes that present with structural limb length discrepancies greater than 4 mm. Travell and Simons (148) are less concerned about the effects of relatively small limb length discrepancies. They recommended a 7 mm structural limb length discrepancy be treated only when it is suspected of being a perpetuating factor in myofascial pain syndromes. Otherwise, it is suggested that heel lifts be used preventively only in the treatment of structural limb length discrepancies exceeding 12 mm or more. As demonstrated by Song et al. (175), even this degree of limb length discrepancy need not be treated with a lift, since these authors demonstrate that limb length discrepancies less than 3% of the length of the longer extremity (approximately 2.25 cm) are not associated with compensatory movement strategies. (Although these numbers seem a bit extreme since discrepancies greater than 6 mm are readily observed during gait analysis as the long limb hip elevates excessively during midstance while walking, see Fig. 4.89).
Because of conflicting research regarding the degree of discrepancy necessary to justify treatment, the use of a lift should be based upon physical examination (i.e., is a compensatory gait pattern visible) and the patient’s symptoms; e.g., strain of the right gluteus medius muscle responds well to a left heel lift, while right sacroiliac pain responds well to a right heel lift. When a limb length discrepancy is clear upon gait evaluation and the location of the symptoms match with the side of the discrepancy, it is suggested that limb length differences greater than 6 mm be treated with the appropriately sized lift. When the limb length discrepancy is associated with compensatory pelvic obliquity and/or asymmetrical muscle tension, manipulation, deep tissue massage and specific home mobilizations are usually necessary to restore mobility and improve muscle function.
Interestingly, it is often the case that incorporating a heel lift to compensate for structural limb length discrepancies in children under the age of 15 results in the complete disappearance of the limb length discrepancy (i.e., limb lengths become equal) after 3-7 months of wear (176). As a result, children should be evaluated at 6-month intervals to determine whether the heel lift is still necessary. Because of problems with shoe fit, it is recommended that heel lifts greater than 9 mm be added to the midsole or heel and not placed inside the shoe. Heel lifts that run the full length of the midsole will prevent contracture and reduce atrophy of the posterior calf musculature, a common problem when elevating the heel alone.
Additionally, to reduce the risk of injury to the contralateral hip flexors and adductors (which are stretched with heel lift), large structural limb length discrepancies should be treated by gradually increasing the size of the heel lift at a rate of approximately 6 mm every 4 weeks. During this break-in period, the rectus femoris, iliopsoas and adductor musculature should be gently stretched to reduce the potential for iatrogenic injury. A primary contraindication for heel lift therapy occurs when the lumbar spine is not laterally flexed toward the structurally short leg. Use of a heel lift in this situation could result in recurrent injury to the lumbosacral spine.
Another contraindication is that a heel lift should never be used to treat a functional limb length discrepancy because the lift does not address the cause of the discrepancy and may even create a unilateral weakness of the involved lower extremity (177). Treatment for a functional limb length discrepancy requires the appropriate manual therapies to address the soft tissue contractures that may be twisting the pelvis and, if necessary, an orthotic to correct asymmetrical pronation that may be causing the limb length discrepancy. In a study in which a combination of custom orthotics and manipulative techniques were used to correct functional limb length discrepancies secondary to asymmetrical pronation and its associated sacroiliac joint dysfunction, Rothbart and Estabrook (158) noted that 78 of the 81 patients treated exhibited a complete reduction in low back pain with 77% of these individuals remaining asymptomatic 6 months after their last manipulative treatment.
The authors related the reduced chronicity to the fact that the orthotics maintained a more functionally efficient posture, thereby allowing even short-term manipulation (i.e., 3 weeks) to have a more permanent effect. Isolating the exact degree of structural vs. functional limb length discrepancy is not always easy and requires careful observation and examination. Before casually recommending a heel lift based upon information obtained from a single ASIS to medial malleolus measurement, the practitioner should have fully evaluated respective tibial and femoral lengths in a variety of positions, checked for soft tissue contracture that might be twisting the pelvis, and carefully evaluated foot function to determine whether asymmetrical subtalar joint motion is contributing to a functional limb length discrepancy.
Prior to prescribing a heel lift, a simple test can be performed during physical examination that is surprisingly helpful for confirming the weight-bearing and off weight-bearing measurements. By having the upright patient shift body weight back and forth between the right and left leg, and asking them to stand on the more comfortable lower extremity, the vast majority of patients will stand on the shorter lower limb, as this levels the lumbar spine and reduces pressure on the chronically overworked long limb hip abductor musculature. If the patient consistently finds it more comfortable to stand on what you have measured to be the longer lower extremity, the decision to incorporate a heel lift should be reconsidered.
References available upon request. Please contact us at HumanLocomotion.com for more information.