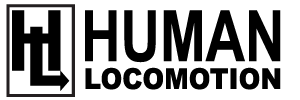
Next to osteoarthritis, greater trochanter pain syndrome is the most frequently encountered hip injury, and it is estimated that it will eventually affect between 10% and 25% of the population (1). The typical patient complains of pain with single-leg stance and the discomfort is often aggravated by sidelying on the affected hip. The lateral hip pain may be reproduced by palpating the lateral and posterior aspects of the greater trochanter, and/or by resisted contraction of the hip abductor/external rotator musculature. The female to male ratio for this condition is 4:1, and 40 to 60 year olds are especially vulnerable. This common condition is surprisingly difficult to treat, and symptoms may last months to years. While it was originally believed the lateral hip pain resulted from chronic inflammation in 1 of the 3 greater trochanter bursae (Fig. 1), recent research confirms that bursal inflammation correlates poorly with the presence of lateral hip pain. As a result, the term greater trochanter bursitis has been abandoned in favor of greater trochanter pain syndrome.
To identify the specific tissues responsible for the development of lateral hip pain, Woodley et al. (2) performed MRI evaluations of the symptomatic and asymptomatic hips in 40 patients presenting with unilateral greater trochanter pain syndrome. After having the MRIs read by 3 radiologists, the authors discovered that although bursal inflammation had no correlation with the presence of lateral hip pain, gluteus medius tendinopathy and atrophy of the gluteus minimus muscle were relatively common and occurred almost exclusively on the side of the symptomatic hip. Because the findings by Woodley et al. (2) are consistent with other research confirming that hip abductor tendinopathy correlates with the presence of greater trochanteric pain syndrome (3), treatment interventions should emphasize restoration of tendon function, not reduction of bursal inflammation.
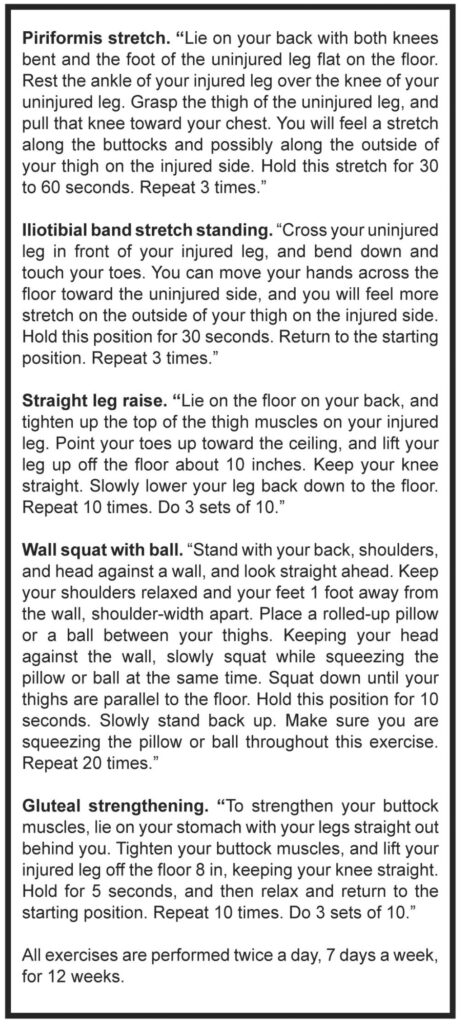
In an important study comparing the efficacy of differ- ent treatment protocols, Rompe et al. (3) assigned 229 patients with refractory unilateral greater trochanter pain syndrome to 1 of 3 different treatment protocols: a single local corticosteroid injection (25 mg prednisolone), a repetitive low-energy shock wave treatment, or a home training program that included specific hip abductor/rotator stretches and exercises (see table 1). Subjects were reevaluated at 1, 4, and 15 months to evaluate the degree of recovery and severity of pain. The results of this study were interesting in that corticosteroid injection produced significant short-term improvements, while shock wave and home stretches/exercises produced better long-term results.
For example, at the 1-month mark, 75% of the subjects receiving corticosteroid injection reported significant reductions in pain, with only 13% of the shock wave and 7% of the home exercise group showing significant pain reductions. However, at the 4-month follow-up, 68% of the individuals receiving radial shock wave presented with significant pain reductions, compared to 51% of the corticosteroid group and 41% of the home stretches and exercises group. By the 15-month follow-up, the home stretching/exercise group had the best outcomes, with 80% reporting significant pain reductions, compared to 74% of the shock wave and 48% of the corticosteroid injection group. The authors state that because the significant short-term superiority of a single corticosteroid injection reversed after 1 month, “the role of corticosteroid injection for greater trochanter pain needs to be reconsidered.”
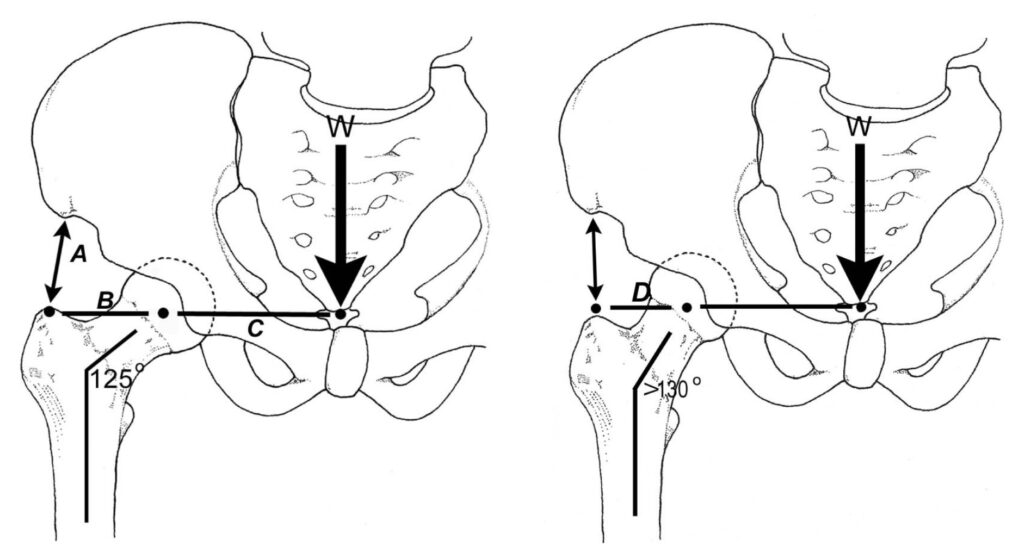
Given the economic cost of shock wave therapy, the simplest and most effective method of treating greater trochanter pain syndrome is with strengthening exercises and stretches. Because the typical greater trochanteric pain syndrome is associated with tendinopathy of glute- us medius and atrophy of gluteus minimus, it is import- ant to isolate these muscles with specific stretches and eccentric exercises (Fig. 2). These exercises are especially helpful when treating individuals with coxa valgum (Fig. 3), since an increased femoral neck angle reduces the mechanical efficiency of the hip abductors and a strong gluteus medius is necessary for injury prevention.
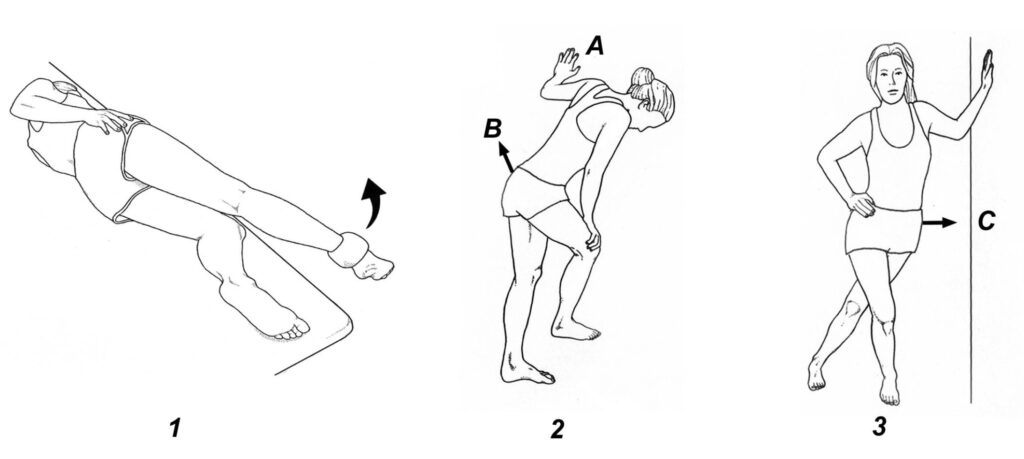
1) Gluteus medius home exercises. The sidelying patient is positioned near the edge of a support surface with the involved hip adducted (i.e., the ankle is lower than the support surface). The posterior fibers of gluteus medius are exercised by raising and lowering the straight lower extremity through a full range of motion (the hip is abducted and adducted approximately 45° in each direction). To strengthen the gluteus minimus, the same maneuver is performed with the involved hip extended, so the straight lower extremity is hanging off the back edge of the support surface. 2) Gluteus medius stretch. The leg you are stretching is positioned behind you, while the hand on that side is resting against a wall (A). To stretch the gluteus medius muscle, move your hip to- wards the wall (B). 3) Gluteus minimus stretch. The involved leg is extended while the pelvis is moved towards the wall (C). Your spine should be kept in a midline position while performing this stretch.
In addition to these exercises, clinical outcomes are often improved by performing deep tissue massage on the hip abductor and external rotator tendons. To access these tendons, it is often necessary to position the supine patient with the hip abducted 45°. In order to produce the best possible outcomes, the practitioner must be able to isolate each specific tendon near its attachment on the greater trochanter (Fig. 1). By coupling eccentric exercises with specific deep tissue massage of the involved tendons, significant reductions in pain occur within the first 4 months of treatment.
References:
- Willaims B, Cohen S. Greater trochanter pain syndrome: a review of anatomy, diagnosis, and treatment. An- esthesia Analgesia. 2009;108:1662.
- Woodley S, Nicholson H, Livingstone V, et al. Lateral hip pain: findings from magnetic resonance imaging and clinical examination. J Orthop Sports Phys Ther. 2008;38:313.
- Rompe J, Segal N, Cachio A, et al. Home training, local corticosteroid injection, or radio shock wave therapy for greater trochanteric pain syndrome. Am J Sports Med. 2009;37:1981.