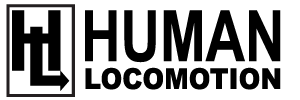
In any given year, nearly one in 100,000 adults will develop a vertebral artery dissection (VAD) (1) (Fig. 1). Factors that increase the risk of dissection include elevated homocysteine levels, Marfan’s syndrome, family history of stroke, migraines, and even seasonal allergies (vertebral artery dissections are more likely to occur in the fall) (2,3). If the initial damage to the lining of the vertebral artery is minor and is left alone, the artery often heals without incident as platelets become adherent to the site of the tear, mix with fibrin and form a “white thrombus” that retracts into the vessel wall (4). With these minor injuries, blood continues to make its way to the brainstem and frequently the only sign the artery is damaged is referred pain from inner lining of the artery to the head and/or neck. To prove that minor damage to the vertebral artery is capable of referring pain, researchers inflated balloons that had been inserted into the vertebral arteries of healthy subjects and noted the stretch induced by the inflating balloons referred pain from the subjects’ foreheads and cheeks to their occiputs, posterior necks, and even upper trapezius muscles (5).
If the inner lining fails to heal, blood, being forced under systolic pressure, may enter the artery wall through the initial tear thereby splitting different layers of the artery, forming a subintimal hematoma or a subadventitial aneurysm. Either way, blood flow through the affected vertebral artery becomes significantly diminished and symptoms related to brainstem infarct often develop. VADs are serious injuries with a two percent mortality rate during the first month, and one percent mortality rate per year for the next 10 years (6). Besides the telltale intense headache so often associated with VAD, a range of ocular disturbances may occur; e.g. diplopia, blurred vision, conjugate gaze paralysis, and/or nystagmus. Additional symptoms associated with vertebral artery dissection are vertigo, slurred speech, difficulty swallowing, nausea/vomiting, and facial and/or extremity paresthesias.
While neurologists are quick to blame the chiropractic profession any time someone suffers a VAD, this is in large part due to the fact that early research showed that a disproportionate number of patients suffering vertebral artery dissection had cervical manipulation within a few days prior to developing their stroke. The temporal connection between chiropractic adjustments and VAD initially seemed to clearly suggest that cervical adjustments, and/or any other vigorous movement of the neck, could damage a vertebral artery causing a healthy vertebral artery to dissect. More recently, researchers are discovering that chiropractic manipulation is not a risk factor for developing vertebral artery dissection (7).
To prove that chiropractic care does not result in an increased risk of VAD, Cassidy et al. (7) evaluated the health records of over 12 million Canadians followed for 9 years. Over that time, there were 818 cases of vertebral/ basilar artery dissection which occurred during 109,020,875 person-years of observation (i.e., 12 million people followed for 9 years). The data was then analyzed to see if there was a higher prevalence of VAD in patients who received chiropractic care compared to conventional medical care (which would have confirmed that chiropractic care was potentially dangerous to the vertebral artery). The final analysis of their data confirmed that although patients with vertebral artery dissections were more likely to seek chiropractic and/or medical care, there was essentially no difference in the development of a vertebral artery dissection whether the patient saw a chiropractor and/or a medical doctor. The results of this study suggest that a damaged vertebral artery produces symptoms that cause the patient to seek medical attention, and that chiropractic care is no more dangerous to the vertebral artery than conventional medical intervention. The authors 2017 follow-up paper on carotid artery dissections also confirmed that chiropractic care is no more likely to result in carotid artery dissection than medical intervention (8).
It must be emphasized that the research by Cassidy et al. (7,8) in no way suggests that a traumatized vertebral artery can tolerate the mechanical stress associated with even gentle manipulation, especially rotational and/or extension manipulation (2). In their conclusion, Cassidy et al. (7) state that it is “possible that chiropractic manipulation, or even simple range of motion examination by any practitioner, could result in a thromboembolic event in a patient with a pre-existing vertebral artery dissection.” The fact that so many people suffer vertebral artery dissection within minutes following excessive neck motions associated with practicing yoga, stargazing, ceiling painting, and even having their hair washed in a beauty salon, confirms that while a healthy vertebral artery is most likely not stressed with even rapid, full-range neck motions, a dissected vertebral artery is most likely structurally weaker and should therefore not be mechanically stressed with upper cervical chiropractic manipulation (9).
This is especially true for upper cervical adjustments incorporating rotation and/or extension. Nearly 20 years ago, I made a case for practitioners to abandon all rotation and/or extension upper cervical manipulations in favor of adjustments incorporating lateral flexion of the upper cervical spine (2). In my experience, upper cervical manipulation incorporating lateral flexion produces the same positive outcomes with a reduced risk of iatrogenic injury. The connection between upper cervical rotation and VAD is supported by the recent finding that 80% of right-handed golfers suffer VAD between the atlas and axis on their right side (10).
Because chiropractic manipulation is significantly safer than the vast majority of medical interventions for managing neck pain (e.g., 1 in 1,200 people who take NSAIDs daily for 2 months will die from gastroduodenal complications [11]), the challenge for our profession is how to identify people with active dissections so they are not manipulated. Since pre-manipulative VAD screening tests such as Maigne’s, George’s, and Wallenberg’s tests have been proven to be useless for identifying at-risk patients prone to vertebral artery dissection, the most important factor in identifying a patient with an active dissection is to pay close attention to their symptoms. According to Terrett (9), the most common symptoms associated with VAD are vertigo and/or headache. While vertigo by itself is generally not indicative of vertebral artery dissection, almost every patient with a VAD reports the associated headache/neck pain is “unlike any pain I have ever experienced before.” This statement is a harbinger of a poor outcome with manipulation as it is a strong indication of a possible VAD.
In addition to subjective complaints, it is imperative that every chiropractor perform a thorough neurological examination of the areas of the brainstem most likely to be affected by VAD (Fig. 2). These tests are listed in Table 1 and, with practice, the full neurological work-up can be performed in minutes. Although vertebral artery dis- sections are rare, the often-catastrophic consequences associated with this difficult to diagnose condition makes thorough evaluation and examination essential.
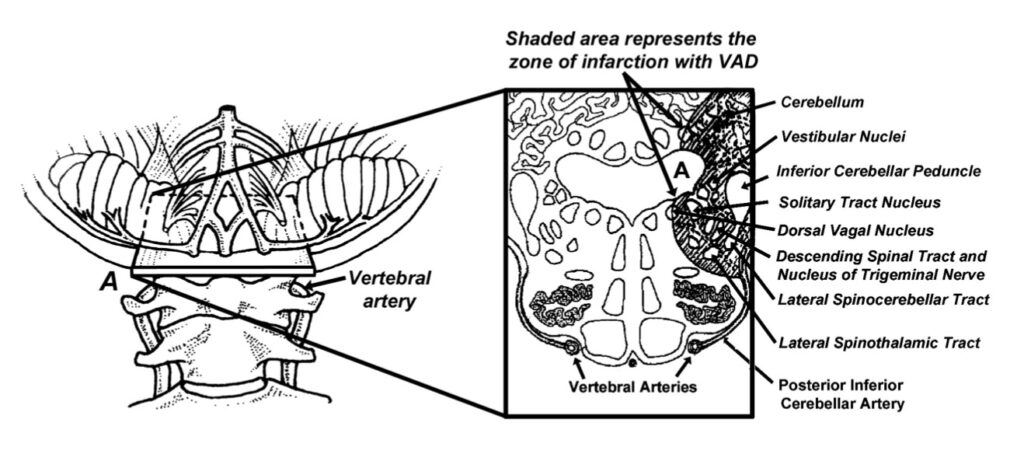
| Affected Tract | Symptoms | Clinical Tests |
|---|---|---|
| Ascending spinal tract and nucleus of trigeminal nerve. | Pain in eye, face, and/or forehead, with ipsilateral loss of pain and temperature sensation in face. | Decreased sensation to light touch and temperature over ipsilateral face. Can be evaluated with cotton swab and/or light brush. |
| Nucleus ambiguous, solitary tract nucleus, and dorsal vagal nucleus. | Difficulty swallowing, palatal paresis, and/or hoarseness. | Observe pallet with “Ahh” and have patient swallow and then whisper. |
| Autonomic fibers. | Eyelid ptosis and extremities often feel cold, with Raynaud’s symptoms. | Check eyelids and pupils for ptosis and/ or miosis. Check skin temp with thermal scanner and look for 4-degree temperature difference between the 2 sides. |
| Vestibular nuclei. | Dizziness, vertigo, and double vision. | Perform Romberg’s test and note ocular movements. Look for horizontal nystagmus. |
| Inferior cerebellar peduncle. | Staggering gait. | Have patient walk and change direction: patients with VAD often shift weight towards the side of lesion, especially when turning around. Also have patient rapidly abduct arms and stop arm motion suddenly: when a VAD is present, the ipsilateral arm is unable to stop smoothly. |
| Lateral spinothalamic tract. | Decreased ability to notice subtle differences in temperature in the extremities and torso. | Place metal ruler over central abdomen and evaluate differences in temperature sensation along the midsagittal bisection. |
| Cerebellum. | Vomiting, headaches, loss of consciousness. | Check single-leg balance with Romberg’s test. |
References:
- Lee VH, Brown RD Jr, Mandrekar JN, et al. Incidence and outcome of cervical artery dissection: a population-based study. Neurology. 2006;67:1809–12.
- Michaud T. Uneventful upper cervical manipulation in the presence of a damaged vertebral artery. J Manip Phys Ther. 2002; 25:472-483.
- Schievink WI, Wijdicks EM, Kuiper JD. Seasonal pattern of spontaneous cervical artery dissection. J Neurosurg. 1998;89:101-3.
- Fields WS. Roll of platelets in arterial thrombosis. In: Netter FH, editor. The Ciba collection of medical illustrations. Vol 1. Princeton, NJ: Ciba Pharmaceutical Company; 1986. p. 52.
- Nicholls FT, Mawad M, Mohr JP et al. Focal headache during balloon inflation in the vertebral and basilar arteries. Headache. 1993; 33:87-89.
- Bassetti C, Carruzzo A, Sturzenegger M, Tuncdogan E. Recurrence of cervical artery dissection. A prospective study of 81 patients. Stroke. 1996;27(10):1804-7.
- Cassidy JD, Boyle E, Côté P, et al., Risk of Vertebrobasilar Stroke and Chiropractic Care, Results of a Population-Based Case-Control and Case-Crossover Study. Spine. 2009; 33:2838-
- Cassidy JD, Boyle E, Côté P, et al. Risk of carotid stroke after chiropractic care: a population-based case-crossover study. J Stroke Cerebrovasc Dis. 2016 Nov 21.
- Terrett AGJ. Current concepts in vertebrobasilar complications following spinal manipulation. West Des Moines, IA:NCMIC Group Inc; 2001.
- Choi M, Hong J, Lee J, et al. Preferential location for arterial dissection presenting as golf-related stroke. Am J Neuroradiology. November 2014; 35:1-4.
- Tramer MR, Moore RA, Reynolds DJM, McQuay HJ. Quantitative estimation of rare adverse events which follow a biological progression: a new model applied to chronic NSAID use. Pain. 2000;85:169-82.