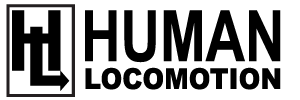
Ankle sprains are surprisingly common. In the United States alone, 23,000 people sprain their ankle each day (Fig. 1). The medical costs associated with treating ankle sprains exceeds $1.1 billion annually (1,2). To make matters worse, these numbers do not take into account the long-term disability often associated with ankle sprains. In a 10-year follow-up of patients suffering ankle sprains, 72% showed signs of arthritis in the ankle joint (3). Given the serious long-term consequences associated with ankle sprains, it is important to know if you’re prone to sprained ankles.
Although numerous factors have been proven to correlate with the development of ankle sprains (such as high arches, poor balance, tight calves, and decreased overall fitness), by far, the best predictors of future ankle sprain are prior ankle sprain and being overweight. In fact, heavy runners with a prior history of ankle sprain are 19 times more likely to suffer another ankle sprain (4). Conversely, a previous ankle sprain can result in impaired coordination and calf tightness that can increase your potential for reinjury. In a three-dimensional study of motion in the foot and ankle while walking, individuals with a prior history of ankle sprain had reduced ground clearance during swing phase and the injured foot was tilted in excessively when it hit the ground (5).
Despite the strong connection between prior sprain and future sprain, there is a counterintuitive inverse relationship between the severity of ligament damage and the potential for reinjury. In a two-year follow-up of 202 elite runners presenting with ankle sprains, researchers from Greece determined that runners with the worst ligament tears had almost a zero percent rate of reinjury, while nearly 20% of runners with less severe ankle sprains were reinjured (6). This study confirms that runners with even mild ankle sprains should be diligent with their ankle rehab. Regardless of the degree of ligament damage, the goal of treating an ankle sprain is to restore strength, flexibility, balance, and endurance as quickly as possible during the first few days following injury. Adding an elastic bandage to a standard air cast has been proven to reduce the length of time to full recovery by 50% (7).
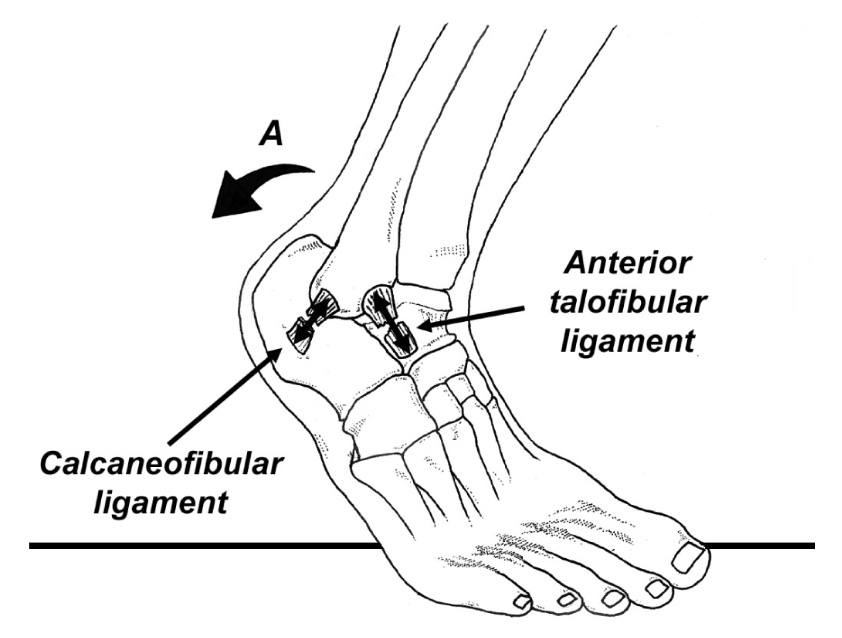
The table below outlines a popular treatment protocol for managing ankle sprains (6), while figure 2 shows an effective tubing exercise that can be performed once symptoms of the acute sprain have resolved.
Treatment Protocol for Managing Ankle Sprains
Phase 1: Runner is unable to bear weight.
- Compressive wrap with U-shaped felt balance around outer ankle. Change every four hours.
- Actively separate your toes for 5 seconds, repeat 10 times.
- Write out the alphabet with the tips of your toes. Repeat five times per day.
- Stationary bike, 15 minutes per day.
- Ankle rock board performed while seated (off weight-bearing), 30 circles, performed clockwise and then counter-clockwise 2 times per day.
Phase 2: The injured runner can walk with minimal discomfort and the sprained ankle has 90 percent full range of motion.
- Stretch all stiff joints in the legs and hips.
- Perform the elastic band exercises illustrated in figure 2; three sets of 25 in each direction.
- Double-leg and then single-leg heel raises on the involved side, three sets of 10 reps, two times per day.
- Standing closed-eye balance, 30 seconds, five times per day.
- Standing single-leg ankle rock board, one minute, five times per day.
Phase 3: You can finally hop on involved ankle without pain.
- Running at 80 percent full speed; avoid forefoot touch-down
- Mini-trampoline; three sets of 30 jumps forward, backward and side to side. Begin on both legs; progress to single-limb
- Plyometrics on a 50 cm and 25 cm box, positioned 1 meter apart. Jump from one box to the ground, then to the other box, landing as softly as possible. Three sets of five reps. Note that this is an advanced drill and should be initially performed with a knowledgeable rehab expert.
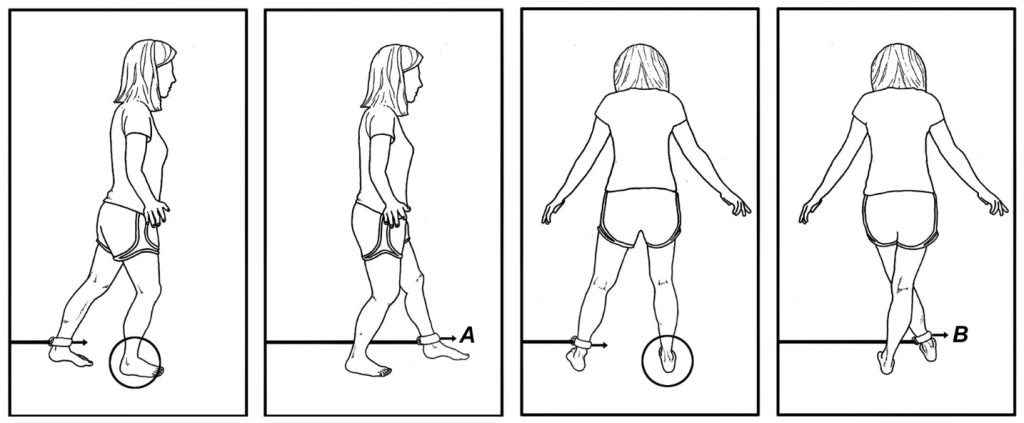
Besides the standard exercise routines, it is also important that problems with balance be addressed. Regularly using an inexpensive foam balance pad can significantly reduce the risk of injury. In one study, there was a 77% decrease in the rate of reinjury when overweight athletes with a prior history of ankle sprain performed balance training on a foam stability pad for five minutes on each leg for four weeks (8). Another study from the Netherlands (9) found that individuals treated with balance board exercises reduced their subsequent reinjury rates by 47%. The improvements in balance can be enhanced by skin taping. As demonstrated by Matsusaka et al. (11), placing a single strip of Kinesiotape along the outer leg and heel while performing balance board training produces more rapid improvements in postural sway (i.e., taped subjects returned to baseline values of postural sway with 6 weeks of training, compared to 8 weeks with balance board training alone). It is also interesting that balance board training on one limb will produce significant improvements in balance on the opposite, untrained limb (295). The cross-training effect associated with balance training allows the injured individual to train the opposite, uninjured leg to enhance balance in the injured leg, even if the injured leg is cast immobilized.
Because foam pads and balance boards do not put your foot through a full range of motion, I recommend using the Two-to- One Ankle Rockboard, which forces your foot to tilt in twice as much as it tilts out (which is how your ankle is designed to move, see figure 3). The board places your foot in the position of a future sprain and then forces you to use your muscles to pull yourself out of the risky position. At first, perform this exercise while seated; after a few days, it can be done while standing. You can watch a video of this rockboard being used at www.humanlocomotion.org. Of course, if you have excessive bruising or swelling you should see your health care provider to make sure nothing is broken. Many inversion sprains result in small fractures that need to be identified prior to initiating a home exercise program.
References:
- McKeon PC, Mattacola CG. Interventions for the prevention of first time and recurrent ankle sprains. Clin Sports Med, 2008;27:371-382.
- Heiderscheit B, Chumanov E, Michalski M, et al. Effects of step rate manipulation on joint mechanics during running. Med Sci Sports Exerc, 2011;43:296-302.
- Verhagen E, van Mechelen W, de Vente W. The effect of preventive measures on the incidence of ankle sprains. Clin J Sport Med, 2000;10:291-296.
- Tyler TF, McHugh MP, Mirabella MR, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med, 2006;34:471-475.
- Delahunt E, Monaghan K, Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in
subjects with functional instability of the ankle joint. Am J Sports Med, 2006;34:1970-1976. - Malliaropoulos N, Ntessalen M, Papacostsa E, et al. Reinjury after acute lateral ankle sprains in elite track and field
athletes. Am J Sports Med, 2009;37:1755. - Beynnon B, Renstrom P, Haugh L, et al. A prospective, randomized clinical investigation of the treatment of first-
time ankle sprains. Am J Sports Med, 2006;34:1401. - McHugh M, Tyler T, Mirabella M, et al. The effectiveness of a balance training intervention in reducing the incidence
of noncontact ankle sprains in high school football players. Am J Sports Med, 2007;35:1289. - Verhagen E, van der Beek A, Twisk J, et al. The effect of proprioceptive balance board training for the prevention
of ankle sprains. Am J Sports Med, 2004;32:1385-1393. - Han K, Ricard M, Fellingham G. Effects of a 4-week exercise program on balance using elastic tubing as a
perturbation force for individuals with a history of ankle sprains. J Orthop Sports Phys Ther. 2009;39:246-255. - Matsusaka N, Yokoyama S, Tsurusaki T, et al. Effect of ankle disk training combined with tactile stimulation to
the leg and foot on functional instability of the ankle. Am J Sports Med. 2001;29:25.