Unlike the hip joint, which possesses a deep ball and socket that provides inherent stability to reduce stress on the restraining ligaments, the knee is particularly prone to injury because the flatness of the tibial plateau provides little protection against excessive motion. This is particularly true when the knee approaches full extension, as the femoral condyles roll forward with little restraint. To protect against hyperextension, most people possess a slight posterior slope of the tibial plateau that increases pressure centered beneath the anterior femoral condyles thereby creating a slight flexion moment that limits hyperextension.
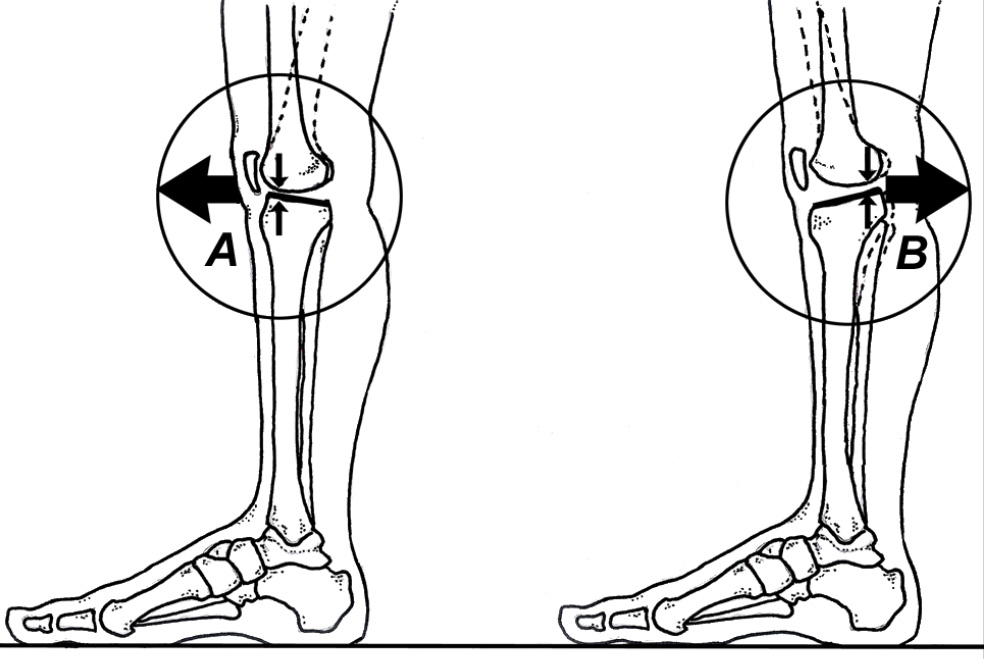
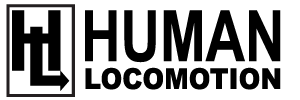
Unfortunately, posterior sloping is not always present and the individual with a horizontal tibial plateau is more dependent upon soft tissue restraining mechanisms (Fig.1). While most authorities claim that a hyperextended knee (also known as genu recurvatum) results from laxity in the cruciate ligaments, collateral ligaments and/or posterior capsule, Morgan et al. prove the posterior oblique ligament provides the most powerful restraint to hyperextension (Fig. 2).
In a cadaveric study in which ligaments were sectioned one at a time and the resultant degree of hyperextension noted, Morgan et al. demonstrate that independent of the order in which ligaments are cut, the greatest increase in knee hyperextension occurs after sectioning the posterior oblique ligament. In fact, the degree of hyperextension following release of the posterior oblique ligament exceeded the degree of hyperextension noted after sectioning the anterior and posterior cruciate ligaments combined.
Often associated with inherited ligamentous laxity, genu recurvatum increases the risk of posterior knee injury during normal gait, particularly when walking on uneven terrain. Hyperextension of the knee is especially troublesome when coupled with genu varum, because it often results in a varus thrust gait in which the entire knee displaces laterally during contact.
To protect against potential injuries associated with genu recurvatum, it is essential the individual learn to walk with the knee slightly flexed throughout stance phase. As demonstrated by Noyes et al., this can be accomplished with gait retraining.
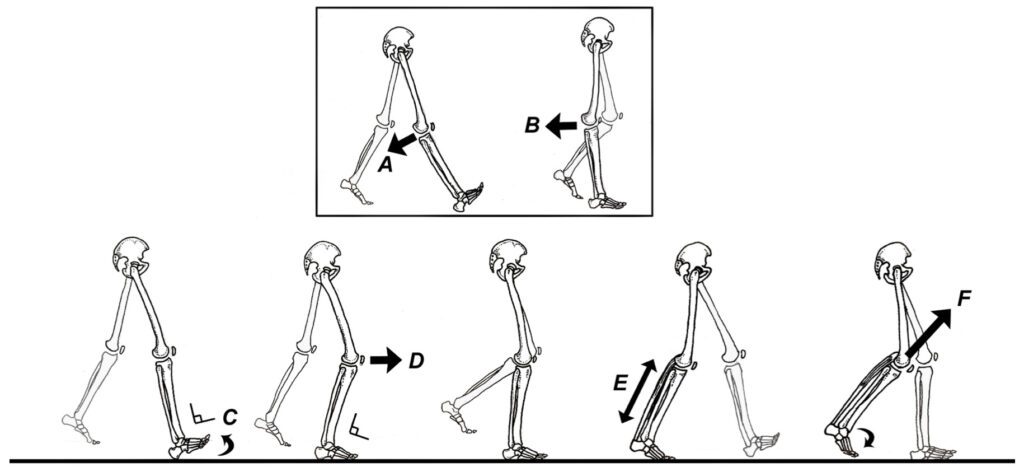
These authors trained 5 patients with symptomatic knee hyperextension/lateral thrust gait patterns to walk while focusing on exaggerating ankle dorsiflexion, maintaining knee flexion and keeping an erect trunk-hip attitude throughout stance phase (Fig. 3).
Follow-up gait and force plate analysis revealed that 4 of the 5 patients significantly reduced the degree of knee hyperextension and improved movement patterns at the hip and ankle. This simple technique of consciously modifying gait restored biomechanics of the hip, knee, and ankle to approximately normal levels of function. The authors emphasize that failure to correct this faulty gait pattern prior to surgical reconstruction would lead to poor clinical outcomes since the abnormal knee motions, if resumed post- operatively, would damage the reconstructed soft tissues.
The clinical implications of this research go far beyond the management of genu recurvatum. By repeating desired movement patterns over and over, you can essentially rewire the CNS and replace faulty motions with safer, more efficient movement patterns. The most common examples of faulty movement pattern occur in valgus collapse of the knee and/or excessive frontal plane hip drop.
Excerpted from Human Locomotion: The Conservative Management of Gait-Related Disorders, by Thomas C. Michaud, DC. For more information, go to HumanLocomotion.com.